Episode Transcript
Written by Alan Helgeson
Randy Preston (guest):
On our refrigerator was a little decal, little magnet saying, “BE FAST. The signs of a stroke.” And she in her brain immediately go, well, he’s disoriented. He’s not speaking properly. He can’t feel his left side. These are all signs of a stroke. Randy, you’re having a stroke. Stay where you are. Turn the car off. We’ll come and get you. We’ll find you.
Courtney Collen (announcer):
This is the “Health and Wellness” podcast brought to you by Sanford Health. Welcome.
The conversation today is all about stroke awareness. Our guests are Dr. Abd Elazim, a neurologist with Sanford Brain and Spine Center in Sioux Falls, South Dakota. And joining Dr. Elazim is Randy Preston, a Sanford Health patient here to share his story. Our host is Alan Helgeson with Sanford Health News.
Alan Helgeson (host):
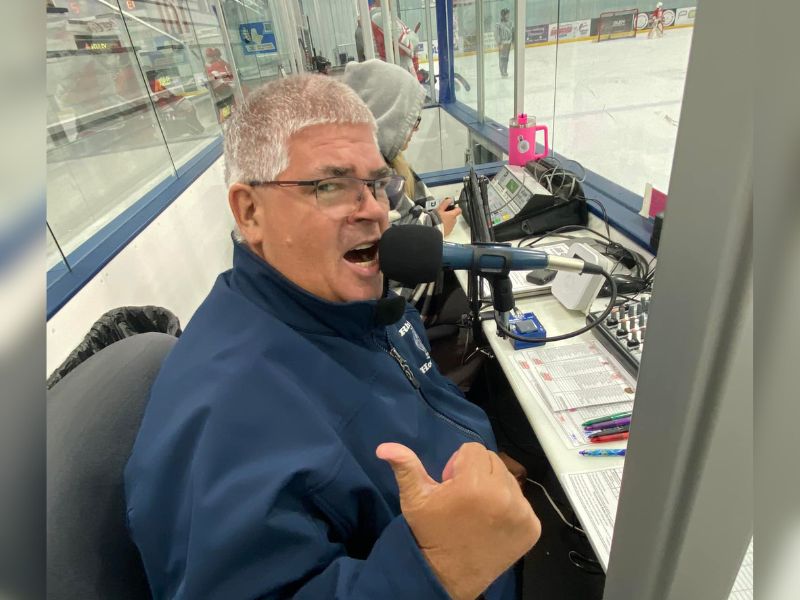
Randy, why don’t you go ahead and say a few things that people might recognize behind the microphone if they were to go to a hockey game here in the Sioux Empire.
Randy Preston:
Ladies and gentlemen, welcome to the ice, your Sioux Falls Stampede!
Alan Helgeson:
And maybe see a baseball game during the summer? They might hear something a little bit different.
Randy Preston:
Ladies and gentlemen, welcome to the Birdcage, home of your Sioux Falls Canaries!
Alan Helgeson:
Now, recently another venue opened up here in Sioux Falls where people could go see collegiate hockey for Augustana.
Randy Preston:
Ladies and gentlemen, welcome to Midco Arena, home of your Augustana Vikings!
Alan Helgeson:
So Randy Preston is not really a stranger to the microphone, so I’m glad you’re here today, but we’re going to talk about something that isn’t something you normally talk about behind that microphone.
Not long ago you came to Sanford Health for a different reason. So let’s go ahead and talk about the day of the stroke and tell us your story of what happened, Randy.
Randy Preston:
Certainly. My wife and I were getting ready to go out on the road. We had some appointments in Fairmont, Minnesota. The entire family was getting ready to leave. So that morning I grabbed the car, filled it with gas, went to the car wash, vacuumed out the car because it was just dirty.
And all of a sudden I started feeling very, very odd. I couldn’t use my left hand, reached up to grab the door handle and it just wouldn’t grab the door handle. Well, this is weird. Well, maybe I, maybe my arm fell asleep while I was vacuuming. Something’s just not quite right. I get in the car, manipulate the car door shut, couldn’t find the seatbelt, tried calling my wife at that point and she didn’t answer the phone. Well, I better get home.
So I backed out of the slot at the car wash, started driving home and on the way home I got lost. And that’s obviously not normal because I drive all the time. Made a left hand turn into a curb instead of turning right onto a street. And at that point I thought, well, OK, this is definitely not normal. I better pull over and try to get ahold of my wife again and find out what’s going on.
Alan Helgeson:
So how much time had passed by this time here, Randy?
Randy Preston:
Less than 10 minutes. This time it was probably five or six minutes and I pulled into a parking lot behind the 18th Amendment in Sioux Falls. It was familiar to me back in the day when I used to drive Lyft and Uber. And that was a good place to stop and get rides. Called my wife and started mumbling through words, telling her, I have no idea where I am. I know where I am, but I can’t, the words won’t come out. And thank goodness for a Life 360 app that we have a locator app. They found me and got me to the – my wife and son both came – my son Trevor grabbed me out of the car, out of the driver’s seat of the car, threw me in the back seat. He got in and basically drove me to the emergency room at Sanford.
I was there within 25 minutes of onset. And at that point I was mumbling through my words. You know, the typical what you hear, the typical stroke thing. I wasn’t able to really communicate very well. Couldn’t feel my left side at all. My left arm, my left leg, none of that was working. My face was drooping. As I go back and look at the dash cam video that I have in my car you can definitely see signs of a stroke, but I didn’t really know what was going on. My wife, when I called her, immediately knew what was happening. And I give all the credit to her for getting me to the hospital as quickly as they did.
Alan Helgeson:
Amazing that they had the quick speed. There were so many things that just aligned to happen right at that time. So how did they know what to do at that time?
Randy Preston:
Well, my wife has been a caretaker for her parents for a number of years. And her dad had a stroke about, oh, I suppose it’s been five or six years ago. And at that point she became involved in a bunch of advocacy groups and some other support groups.
And on our refrigerator was a little decal, little magnet saying, “BE FAST. The signs of a stroke.” And she in her brain immediately go, well, he’s disoriented. He’s not speaking properly. He can’t feel his left side. These are all signs of a stroke. Randy, you’re having a stroke. Stay where you are. Turn the car off. We’ll come and get you. We’ll find you.
And that was ultimately how this, how it all happened.
Alan Helgeson:
Thank goodness that recognizing those signs and symptoms, really one of those big things in the awareness of somebody possibly having a stroke.
I want to turn now to Dr. Abd Elazim, and he was one of the physicians that at the time was part of your care team. And doctor, can we talk about when Randy came to Sanford? Can we talk a little bit about that time and when you may have entered into his care team? Let’s talk about what went on that day.
Dr. Ahmed Abd Elazim:
Certainly. So Randy came to us as a level one stroke alert, and what we mean by level one stroke alert that someone who comes into the hospital, the stroke symptoms or signs very early on in the window for an intervention. And what I mean by intervention is being a candidate for a clot busting medication and an intervention to do a thrombectomy or pulling out a blood clot from the brain.
So he came to us with stroke symptoms and signs in the form of left sided weakness with the left-sided facial droop, left sided upper and lower extremity weakness. And since we lost on the left side, certainly that was very concerning for a stroke.
Alan Helgeson:
So when he came in seeing those signs, now they brought him into the emergency department at Sanford. Is that normally what a person would do if they see something like that?
Dr. Ahmed Abd Elazim:
Correct. So going to the emergency department is the first thing. Anyone with a stroke symptoms and signs should do, calling 911 immediately or going to the ER immediately. Every minute counts.
Alan Helgeson:
I’ve heard a statement, “time is brain.” Can you explain that?
Dr. Ahmed Abd Elazim:
Absolutely. So time is brain in the sense of the sooner an intervention can be done for a stroke patient, the better the outcome is. If you can imagine every minute in a stroke about 1.9 million neurons or brain cells die if we do not do an intervention. So really time is very critical here to improve the outcome by doing an intervention to dissolve the blood clot.
Alan Helgeson:
By that time, his wife and his son getting him here so soon and the ER team knowing that, that’s what really helped him and the positive outcome that he had. Right?
Dr. Ahmed Abd Elazim:
Absolutely.
Alan Helgeson:
So at what point do you come in and do they say, doctor, we want to bring in your expertise as part of the ER care team for a stroke? How does that happen?
Dr. Ahmed Abd Elazim:
So once a stroke patient comes to the ER, a stroke code gets activated and stroke team responds immediately to the ER for an evaluation. The first thing we do is we take quick history, know the exact last known, well, perform a detailed stroke examination and review the brain scans. And based on these results, we’ll take a decision about what to do next.
Alan Helgeson:
Doctor, let’s talk a little bit about you and your team and your expertise and why you are brought in as part of the care team for treating strokes.
Dr. Ahmed Abd Elazim:
We are a stroke team by training. So we are specialized in treating stroke patients. So we do have the capabilities of evaluating the stroke patients and make decisions about giving clot busting medication and doing an intervention to remove a blood clot from the brain and reversing the stroke symptoms on time.
Alan Helgeson:
Let’s talk about those signs and symptoms because we know there are people out there that are maybe not knowing what to look for. So can you share those with us?
Dr. Ahmed Abd Elazim:
Absolutely. So like Mr. Randy said BE FAST. Every letter is specific for certain stroke symptoms or sign. If any of these symptoms or signs happens, we always say, please call 911 or go to the ER immediately.
So B stands for any balance problems that is of a sudden onset.
E for eye, any visual problems like losing one side of the visual field or seeing double or losing vision in one eye.
F for face if there is any facial drooping.
A for arm or leg weakness or numbness.
S for speech, if there is hard time finding words, unable to speak, frustrated because you can’t just find the word that you want to say or if your speech doesn’t make sense, you cannot understand people and people cannot understand you. Or if there is a slurred speech.
T stands for time is brain. If any of these symptoms or signs happen, call 911 or go to the ER immediately. Because we always say time is brain. The sooner you come to the hospital, the more we can offer to reverse the stroke symptoms.
Alan Helgeson:
Now I want to be clear on this too. It’s not that a person has to have all of these symptoms.
Dr. Ahmed Abd Elazim:
Correct. Any of these symptoms.
Alan Helgeson:
Let’s move on to risk factors. We hear with a lot of medical conditions that sometimes things can be more likely to happen if we have certain risk factors. Can you go into some of those?
Dr. Ahmed Abd Elazim:
Certainly. High blood pressure, diabetes, high cholesterol level, smoking, age, also a heart problem called atrial fibrillation. All these are known stroke risk factors.
Alan Helgeson:
Is there anything regarding heredity, history, family history that can bring up some stroke risk factors at all?
Dr. Ahmed Abd Elazim:
So family history of the risk factor we just talked about might be an alarming sign. For example, family history of stroke, previous stroke, family history of high blood pressure, family history of diabetes, all these medical problems that run in family could be an alarming sign for those who have these symptoms or signs.
Alan Helgeson:
Now I wanted to ask you too, now that Randy’s had a stroke and for other people that may have had a stroke, is there more heightened risk of a follow-up stroke or are things just going back to normal if he’s taking care of normal preventive care now?
Dr. Ahmed Abd Elazim:
Whenever we see a stroke, there are really two questions that we try to answer. The first question is, why did that stroke happen? And by understanding this question, we can answer the second question, how can we prevent another stroke from happening in the future? And this is really when the stroke expertise come to play.
So for Mr. Randy, we worked hard to figure out why did the stroke happen in order to place him on the right treatment to prevent another stroke from happening in the future. And by understanding why the stroke happened, we certainly can prevent future strokes from happening again by putting the patient on the right treatment.
Alan Helgeson:
Well, we’re so glad that Randy had such a positive outcome here and that he’s sitting here today and telling his story because I’ve known Randy for a long time. And I know Randy, you’re going to be (laugh) telling everybody, go out and be aware and know these signs and symptoms, right?
Randy Preston:
That’s correct. Be aware, know the signs and symptoms. BE FAST (laugh) and honestly, don’t be scared of asking the questions. You know, don’t be scared of running yourself into the into the ER If you have any symptoms at all. It’s much better to be safe than sorry. I don’t want to say I’m a living proof of that, but you know, my father had a stroke several years ago before he passed away and he was never the same after he – and he didn’t get it treated properly. It took him two and a half hours to get to the ER. So it was a whole different, a whole different outcome.
Alan Helgeson:
Randy was very fortunate living in Sioux Falls, 25 minutes getting to the ER. But for listeners that may live in some of the more rural remote parts, if that happens, what can we share with them and how is Sanford connected to care for those patients in that same way?
Dr. Ahmed Abd Elazim:
So same thing applies, call 911 or go to your local ER immediately. We have the capability of connecting to remote ER and other remote facilities and do what we call a telestroke. So if there is a stroke case in these remote areas, they can connect to the camera, have me on board, look at the patient immediately on the camera, and make decisions also to treat the stroke case.
Alan Helgeson:
That’s fantastic, fantastic. Connected care regardless of where you are.
Dr. Ahmed Abd Elazim:
Exactly.
Alan Helgeson:
So good to know that. And that’s really comforting for people regardless of where you live —
Dr. Ahmed Abd Elazim:
Absolutely.
Alan Helgeson:
— to have that kind of care. What’s that one takeaway you’d like people to take away from this today about stroke?
Dr. Ahmed Abd Elazim:
Time is brain. If you have any stroke symptoms or sign, please remember the BE FAST acronym and go to the ER or call 911 immediately.
Alan Helgeson:
Randy, how about you?
Randy Preston:
I’ll put it in my own personal perspective because I’m the kind of guy that will just suck it up and not bother other people. Don’t worry about it. If you see any signs, get yourself to the ER immediately. Don’t suck it up.
Alan Helgeson:
I want to thank you both for being part of this podcast. Randy Preston, thank you for sharing your story with us today. Dr. Abd Elazim, a neurologist with Sanford Health, we appreciate you taking your time today.
Courtney Collen:
This episode is part of the “Health and Wellness” series by Sanford Health. For more from Sanford Health, find us on Apple, Spotify and news.sanfordhealth.org.
Get more episodes in this series
…
Posted In Brain & Spine, Emergency Medicine, Healthy Living, Heart, Internal Medicine, Neurology, Rural Health, Sioux Falls, Specialty Care, Symptom Management, Vascular