Tarah Heupel is no stranger to seeing signs.
Although she lives in Aberdeen, South Dakota, her job with Sanford Health marketing takes her to Sioux Falls from time to time. That three-hour drive comes with some familiar checkpoints.
“When I get to Watertown, that’s the halfway point. And then once you get off at Summit, it’s a quiet drive for about an hour,” said Heupel.
But some signs are more important than others, like in March of 2024, when Heupel was in Sioux Falls for work and started feeling unwell.
“Something just felt off. I was a little lightheaded, a little bit nauseous. Something just didn’t feel right,” said Heupel, who initially chalked up her symptoms to anxiety. “By the second morning, I woke up and I could feel pain radiating down my arm. I could feel my heartbeat in my wrist and my elbow and my shoulder. I think that’s when things started to get serious for me.”
Heupel went home to Aberdeen and reached out to her primary care provider. Face to face, it was clear something else was at the root of her symptoms.
“She looked fatigued. She looked like she didn’t feel well,” said Sanford Health advanced practice nurse Natalie Braun. “She had classic signs of a heart etiology that we were kind of looking at, so it didn’t fit for me for anxiety.”
An EKG would show that Heupel was experiencing a spontaneous coronary artery dissection – or SCAD.
What is SCAD?
SCAD is a rare disease where the artery wall splits in two.
“It’s like when you have an onion, and you split the onion,” said Marian Petrasko, M.D., an interventional cardiologist at the Sanford Cardiovascular Institute in Sioux Falls.
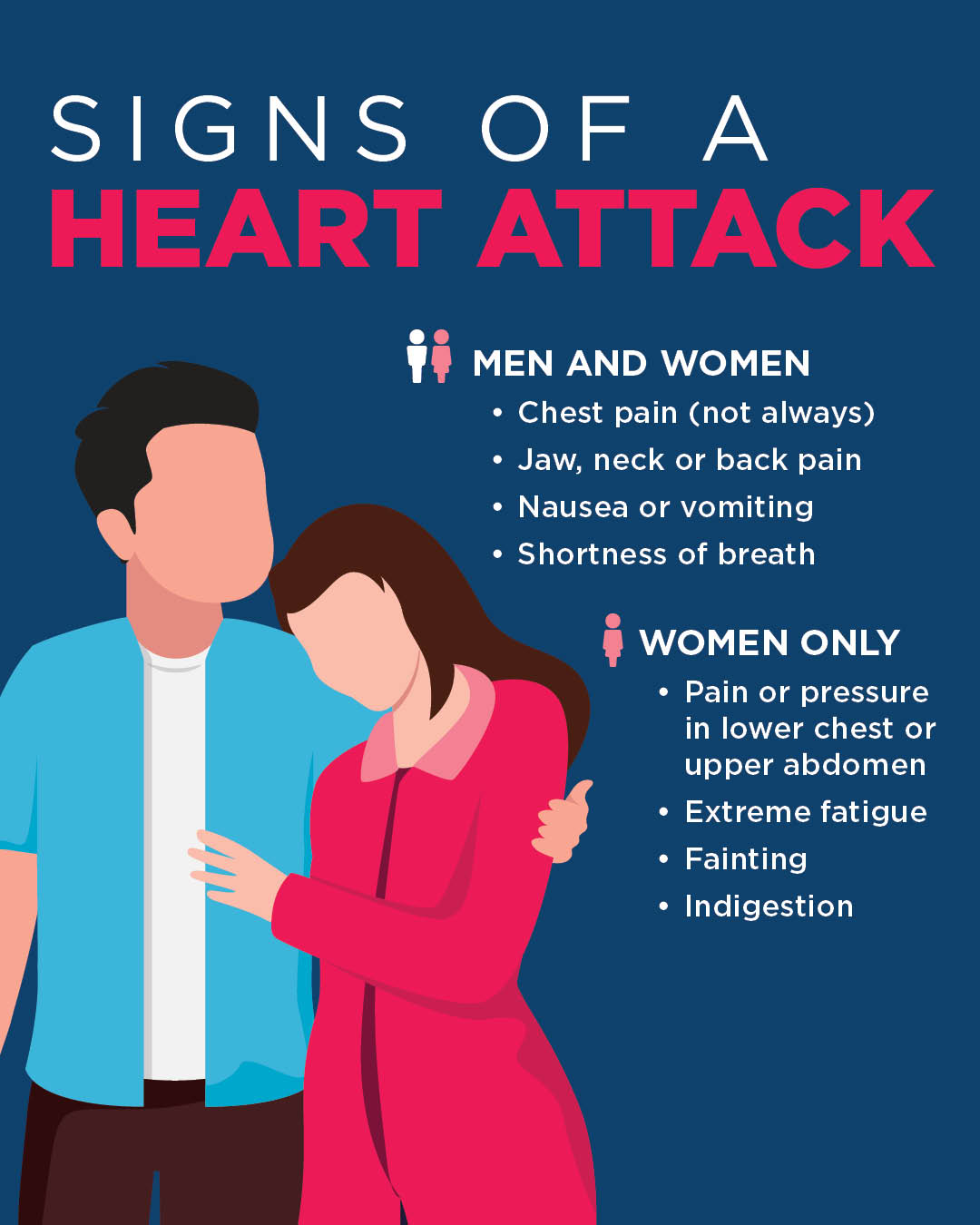
SCAD symptoms are similar to a heart attack:
- Chest pain
- Sweats
- Nausea
- Shortness of breath
Enlarge

Signs of a heart attack. Graphic by Kris Hedrick, Sanford Health
The cause remains unclear, partly because of how rarely it’s diagnosed. SCAD accounts for less than 1% of heart attack cases or acute coronary syndrome.
It’s also difficult to predict. Roughly 85% of SCAD patients are women, predominantly women in their 40s and 50s. According to the American Heart Association, patients are usually postpartum or postmenopausal women who are otherwise healthy.
“It’s one of those diseases that is infrequent, so we don’t have as much knowledge about it,” said Petrasko. “A large portion of the patients, we don’t find a reason for it.”
‘We’re going now’
Heupel’s EKG provided a jumping off point for her cardiac care team.
“I ran to our cardiology department – we’re rural, so it’s literally next door – and I said to the cardiologist, ‘I think I have either a dissection or a heart attack,’” said Braun. “I kind of just threw up the EKG and his eyes got big.”
Heupel heard the call over the building’s intercom for a “hot heart” – a message for a possible heart attack – but didn’t think it was for her. She also didn’t know one of her arteries was completely blocked.
“I could hear this flurry of activity outside the room,” said Heupel, “and all of a sudden, the door opens and they’re there with a wheelchair, and they’re like, ‘We’re going now.’”
Heupel spent two days in the hospital as the cardiac care team treated her SCAD with medication. During that time, staff discovered another problem – Heupel was bleeding internally.
“At that point, that’s when they decided to transfer me to the heart hospital in Sioux Falls,” said Heupel. “It was an incredibly scary thing to experience. It took a long time to realize that this was actually happening. There really was something wrong and something serious was happening.”
Heupel was admitted to the Sanford Heart Hospital on a Thursday and discharged by Sunday.

Photo courtesy of Tarah Heupel
“Everyone who was involved in my care – from the primary care provider that initially ran the EKG to her nurse, my cardiology team, my cardiac rehab team after the fact – every step of the journey has been this incredible family that’s been behind me,” said Heupel.
Patient-provider relationship
After six weeks of rest and recovery, Heupel started feeling like herself again.
“Thankfully, I’ve gotten to a really great place where it really hasn’t changed that much for me at this point,” said Heupel, a mother of three. “After doing cardiac rehab, I got back to a spot where I could feel comfortable exercising again. I feel a lot more confident in what my body can and can’t do.”
Heupel credits her road to recovery to a cardiac care team, which started with her primary care provider.
“If you do develop that relationship with the provider, and stick with the same provider, there is benefit. The benefit of this was she does not have anxiety, she does not have these symptoms that she’s talking herself into,” said Braun. “I know her. It saves time because I don’t have to sift through her history.”
In emergencies like this, time becomes more crucial by the minute.
“The earlier you start to treat a heart attack, every minute literally saves some minuscule part of the heart,” said Dr. Petrasko.
For Heupel, her SCAD was a reminder to listen to her body. She’s encouraging others to do the same.
“You know when something’s not right and to follow your gut and to just go get it checked out,” said Heupel. “There have been so many moments in the last year that I’ve just kind of stopped and been so grateful that I’m still here, and that I get to experience these things with my family and my friends, and I get to keep living a very normal life. I’m incredibly grateful for that.”
Learn more
- What does a heart attack feel like?
- Yoga instructor’s scare an example of heart attack in women
- Heart attack survivor almost missed the warning signs
…
Posted In Aberdeen, Emergency Medicine, Family Medicine, Heart, Sioux Falls