Episode Transcript
Courtney Collen (Host): Hello. Welcome to One in Eight, a new podcast series brought to you by Sanford Health. I’m your host, Courtney Collen with Sanford Health News. We are really looking forward to kicking off this series all about breast cancer awareness because – and we can’t stress this enough – one in eight women will be diagnosed with breast cancer during her lifetime. Today, we’re talking with Dr. Christina Tello-Skjerseth, a radiologist at Sanford Health in Bismarck, North Dakota. Our topic is all about that breast cancer screening exam: the mammogram. Some common myths misconceptions, and those most-asked questions. Dr. Tello-Skjerseth, thank you so much for being with us.
Dr. Christina Tello-Skjerseth (Guest): Thank you for the opportunity. I’m very happy to be here.
Host: One in eight… that’s a lot of women, isn’t it?
Dr. Christina Tello-Skjerseth (Guest): It is a lot of women. You know, breast cancer is the most commonly-diagnosed cancer in women. And like you said, it affects one in eight women in their lifetime. And more specifically, one in six of those cancers will actually happen in women in their 40s. So I’d really like to stress the importance of mammography for women in their 40s.
Host: To kick things off… Tell us about yourself and your role in Bismarck.
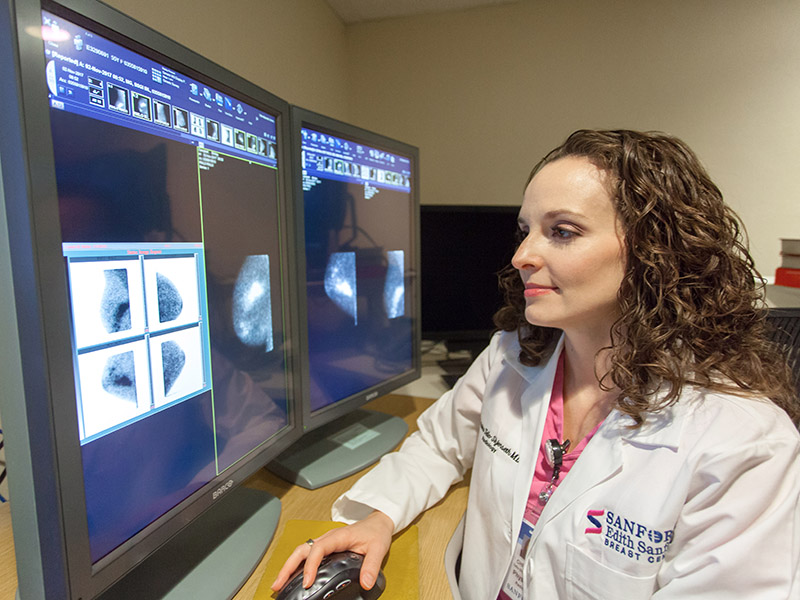
Dr. Christina Tello-Skjerseth (Guest): Sure. Well, um, as you said, I’m a radiologist here at Sanford Bismarck. I was born and raised in Bismarck, North Dakota. So I know the community well, I know the health system well and I know our region very well. I did my training at the University of North Dakota, the medical school there. And then I did my radiology residency at Mayo Clinic in Rochester, Minnesota, which was just a wonderful place to train. And I was very happy to be able to come back to my hometown and provide quality care for the people here.
Here at Sanford, I’m actually the chair of the radiology department. I’m also the lead interpreting physician for our breast imaging department.
Host: What do you most enjoy about being a part of the Sanford Health community?
Dr. Christina Tello-Skjerseth (Guest): Well, one thing I, you know, again, like I mentioned before, being able to have the opportunity to come home to my hometown and treat the people here in this community. I absolutely love working in Bismarck. This is a great place to live a great place to work wonderful people, and I’m very happy to be able to provide that quality care for them… and for Sanford, for giving me that opportunity. As far as Sanford itself, it’s such a wonderful place to work. We have multiple specialists that you wouldn’t expect in this area of the country. I mean, we’re, we’re seen as pretty remote, but we have wonderful specialists that all of our sites and working together as one enterprise, we’re able to have a multidisciplinary approach to treat cancer patients, which is pretty unique in this area of the country.
Host: That’s why we’re so thankful to have you and your team and to be able to have this conversation because year after year, it gets more prevalent and it’s so important to talk about breast cancer and spreading that awareness. So let’s talk about the screening. What is a mammogram?
Dr. Tello-Sjkerseth: I think the important thing to stress here is that we’re doing a screening exam, just like you said. So a screening exam means the patient does not have any symptoms. They’re not having breast pain or a breast lump or any other problem they’re completely asymptomatic. And they’re coming in for an exam that helps us find those early small cancers. So, a mammogram is a specific type of breast cancer screening that we do. And it’s essentially an x-ray of the breast of very specific high-resolution x-ray of the breast that helps us look at the tissue and find little things that can make us suspect a cancer is growing there. So very important as the first step.
Host: What is the recommend at age to get that first mammogram screening?
Dr. Tello-Sjkerseth: There are lots of differing guidelines out there that have come out from various national organizations. Today, I would like to stress the importance of starting annual mammography beginning at age 40. So when you’re 40 years old, you start getting a mammogram and you do it every year as long as you’re healthy. And you would do some kind of treatment if we did find breast cancer, The reason that’s so important is because there has been decades and decades of research showing that annual mammography starting at age 40 has the greatest mortality reduction, meaning it reduces the number of deaths that you can attribute to breast cancer. That’s why it’s so important. Now, some of these other guidelines have come out such as the American Cancer Society or the United States Preventative Services Task Force saying that we should delay that start either to age 45 or 50, and maybe only go every two years.
But I really want to stress the importance today that beginning at age 40 and starting every year is the way to go because, like I said, it has the greatest reduction in breast cancer deaths. And these other societies that have different guidelines still acknowledge that. Their guidelines do say ‘yes, we do agree that the most lives will be saved if you start at age 40 and have it every year’. But some of these other guidelines are basing their recommendations on old data that came out in, in the 80s and 90s when we don’t have, you know, the most recent type of a mammography screening. So our technology is much better. They also are looking more so at the harms than the benefits. So the benefit of annual mammography is like I said, breast cancer reduction, right? We can catch it early. We can treat it early. It’s less aggressive. We can use less aggressive therapies. Now, the harms of mammography that some of these guidelines are stressing include patient anxiety or patient morbidity, meaning they have to have more views or an ultrasound or a biopsy. They also say that radiation can be a harm. The radiation dose is extremely low – it’s essentially negligible. The other thing that they stress as a harm is over-diagnosis, which means that the breast cancer we find would not have resulted in the patient’s death. So, they may die from something else. But the problem with that is we don’t know what cancers will eventually cause death in a patient. There’s no way for us to know that. And just because the patient has a breast cancer, if we find at age 40, it’s going to be earlier and we can catch it and treat it effectively. It’s still going to be there. If they’re age 50 or 45, we just catch it later. So it’s not really over-diagnosis, we’re still finding it, but we’ll find it when they’re 50, instead of 40, the problem with that is it could be more aggressive and then it actually could lead to death in the patient.
So that’s kind of the controversy that we’re facing right now with mammographic screening. I also want to stress that some of these other organizations do not have any specific breast cancer specialists on their panels making these decisions. The organizations that recommend beginning at age 40 and doing it every year are the organizations that are specialists in breast cancer screening, like the American College of Radiology or the American Society of Breast Cancer Surgeons, or the American college of Obstetrics and Gynecology or some of these National Cancer Societies that actually have those specialists on the panels, making these decisions. So that’s why I think it’s better for us to follow those guidelines.
Host: So age 40 every year, would you suggest the same time every year? Would you suggest a certain time of year to get this done?
Dr. Tello-Sjkerseth: Well, the reason why we do it annually is because insurance will cover it if you get one a year and they mean that pretty specific. So if you’re getting it January 1st, you need to wait until at least January 1st, the next year… you can’t get a December 31st or they’re not going to pay for it. Now, now this is just screening mammography. If you have a breast problem, that’s not considered screening, then it turns into a diagnostic mammogram. And that kind of goes down a different route. But we’re just talking about screening. It really doesn’t matter what time of year you get it done. But as long as you get it done, at least once a year and it’s 365 days later, then insurance has no problem covering that. I also want to stress that insurance will cover it starting at age 40 every year, even though there’s different guidelines out there.
Host: I’ve heard a lot of women that make it an annual event around their birthday, Mother’s Day or some significant date. It’s special to them because they know how important it is to get this done.
Dr. Tello-Sjkerseth: Absolutely. I actually do it on my birthday every year. And so does my mother. Well, plus then you kind of remember every year, Oh, it’s my birthday time for my mammogram or, you know, some type of special event that helps you remember because sometimes your, your provider may not remember that you’re due. So it’s important for you to be on top of that.
Host: What’s the difference between a mammogram and, say, a breast self exam. And what are some of the advantages that a mammogram has over any other type of breast cancer screening?
Dr. Tello-Sjkerseth: A mammogram, like I said, is a special type of x-ray of the breast. So we’re seeing the tissue inside the breast. A clinical breast exam either by the patient themselves or by a physician or another provider is when you’re actually examining the breast on the outside and feeling what may be going on in the inside. So you’re looking at the skin, the nipple, is there any, you know, change in coloration? Is there a rash? Is there any puckering of the skin? Is there any thickening? And then of course you feel for lumps or if there’s areas of pain or anything, you know, coming out of the nipple that normally shouldn’t. So, things we may not necessarily see on the mammogram or the x-ray the breast. Now, that’s also very important. It’s very important for women to know what their breasts look and feel like normally. So they’ll know if something becomes abnormal, then they can go to their provider and say, ‘you know what? My breast is is I’m a little different this month. I feel a lump or there I’m getting new pain here, or one is looking a little different than the other’. That brings the attention to something that could be going on underneath. Now. Like I said, that’s the important part is to know about what your breasts look and feel like, but equally important is getting that insight image or that x-ray of the breast. So we can actually see what the tissue is doing. Is there a mass growing in there? Are there calcifications growing in those breast ducts that could become cancer? Those are things we look for on the x-ray part of it
Host: Let’s walk through the mammogram screening and what a woman can expect when she arrives for her appointment.
Dr. Tello-Sjkerseth: Sure. You’ll go through all the normal steps. Just like any other doctor visit, you’ll go through registration. And then you come down to the radiology department, depending on where you’re getting it done. You’ll change into a gown. And then one of our special x-ray technicians called the mammography technician. This is a specialization within a radiology. These techs are specifically trained to do mammography. They’re also certified in it most of the time. They’ll walk you back to our room that has our special mammography extra unit. And then you’ll take one arm out of your gown and place one breast up on our special unit here. And then there is a clear, almost plastic plate that comes down and compresses the breast in two different views. One is an up and down view. So, it’s four images that you take it, it can be painful, you know, it’s very dependent on, on the woman. Sometimes it’s just a little discomfort. Sometimes it’s, it’s pretty exquisitely painful. Sometimes you can have a little nipple discharge with it. And like I said, everyone’s a little bit different, but most patients will just say it’s a little uncomfortable. They may have to push our squeeze a little bit harder depending on if there’s motion. The reason we do that squishing or the compression is so the breast stays still. So we don’t have any motion artifact on the images. So us as radiologists can see everything in the breast really, really well. So once you do both sides, you put the gown back on and then you’re done and you can go home. The whole thing takes maybe 15 minutes. I mean, it’s very scary. It’s a very high-anxiety type of exam. Most women are, you know, concerned about having breast cancer at time. They come in for their mammogram and they just want it to be over before they even get here. And some are too scared to even come in and get it because they’re worried about what we’re going to find, but, rest assured I mean, overall, there’s a very low chance of having breast cancer as a whole. The vast majority of mammograms are going to be benign. Even if you do get called back for something, let’s say we see a little abnormality on your screening mammogram, and you get a call back that usually sends the women into a pretty high anxiety state. They already assume they have cancer. That’s not the case. The vast majority though is probably 90% of those cases that we call back turn out to be benign. It’s just that we want a couple more extra images to make sure we’re not missing something.
Host: As a physician, what are some of those common questions that you get about the mammogram screening or some of the conversations that you have with patients or friends, women in your life when it comes to getting that mammogram?
Dr. Tello-Sjkerseth: Absolutely. Yeah, that’s the number one question: is it going to hurt? And normally I say, well, yes, it’s uncomfortable, but I guarantee you getting a breast cancer and having to go through that treatment is probably going to be way more painful than the mammogram. I should also say it can be more painful depending on if you’re currently having your menstrual cycle. So, some women may actually time it with their cycle so it’s not during that time of the month when their breast is more sensitive. Pain is a big question. Another question I get all the time is about the radiation and about how ‘well I’ve heard x-rays can cause cancer. And I’ve heard the radiation dose is really high’. It’s not, it’s very, very low. We have new technologies coming out all the time that decrease the radiation dose. The radiation dose from having a standard screening mammographic exam is about equal to the amount of radiation you’re going to get just from living on planet earth for about three months. It’s very similar to a chest x-ray dose. So it’s really very, very low dose. It’s essentially negligible. I also stress that all of this, you know, so-called radiation data we have and how it produces cancers. That’s all based from data from the atomic bomb survivors. So it’s all extrapolated data from all those early studies.
Another question we get a lot is, ‘well, I have dense breasts. I heard mammograms. Aren’t really good with dense breasts’ and you know, the answer to that is kind of ‘yes’ and ‘no’. Mammograms are always the gold standard. Like I said, they’re the only screening tests we have that has shown that reduction breast cancer deaths. Now in women with dense breasts, the sensitivity of mammograms to pick up the cancer, it does drop pretty significantly sometimes by 50%. So that’s why we still do the mammograms, but we offer supplemental screening usually for those women such as 3D mammography. I’m sure most women have heard of that by now. And that’s actually becoming standard of care. So here at Sanford, we do probably 90% or more of our patients get that 3D mammogram, which gives us an even better look at the tissue and makes dense breasts a little easier for us to see through. So even though you have dense breasts, you should still get your mammogram. We can still see some things on mammogram, especially those little tiny calcifications. That’s really the only modality we have that sees those calcifications really, really well. So we want to stress the importance of getting that, even though you do have dense breasts, you may have to get another exam with it, but you’re still getting that gold standard.
Another question I get is, well, ‘if I get a call back, does that mean I have cancer?’ And when I say call back, that means we’re, we’re calling you and saying, we want you to come back and have some extra views… That does not mean you have cancer. It causes a lot of high anxiety and I totally understand that, but like I said earlier, it’s a very, very small percentage of those patients that could get a call back that actually have the cancer. So it’s okay. If you get the call back, most women have had at least one in their lifetime. Some of them get them every year. It’s just something you have to kind of work through and, you know, stay calm and just realize once it gets to the point where we’re really worried, we’re going to let you know, and we’ll talk you through it.
Host: You had mentioned the 3D mammography screening. Are there any other types of mammography screenings? And does it depend on the woman, the type of screening that she will undergo?
Dr. Tello-Sjkerseth: Yes, that’s a great question. So, as far as mammography, we have our regular, you know, we say 2-D or traditional screening mammography, which is being replaced with 3D mammography or Tomosynthesis. That’s the other word for it. So those are the types of essentially x-rays of the breast that we use to screen for mammograms. Now, there are other types of breast cancer screening, such as breast MRI. That’s not a mammogram that is an exam that uses essentially magnets to help us look at the breast tissue. It gives us a much better look at what’s going on. We can also see your lymph nodes. We can see your chest wall. We can see part of your lungs and your liver. It’s a very, very sensitive tool, meaning that it’s going to find that breast cancer, if you have it. It’s better than mammography. And we reserve that for high-risk women because it’s very, very expensive and insurance is not going to cover it for the general population. A breast MRI can be up to $4,000. Women don’t want to pay that. A mammogram can be anywhere from $200 to $300. And so obviously insurance wants to cover the mammogram. So MRI is reserved for the very high-risk women that need that extra screening. The other type of breast imaging cancer screening tool we have is ultrasound. That’s another supplemental tool that we offer women that have dense breasts. So some women will get a mammogram and that whole breast ultrasound at the same time just to give us a little extra look inside and to see if we’re missing anything that we would have not seen on the mammogram. Those are the main types of screening. There are some other ones out there you may have heard of such as a gamma gram, which is like a BSGI or MBI there’s a contrast-enhanced mammogram, which is kind of like what, what you would get during a cat scan or a CT scan, where we inject a dye into your IV and then things in the breast might light up and we can see things better. So there’s, there’s lots of other modalities out there to screen the breasts, but the big one is your annual screening mammograms.
Host: Great. So what are some other common questions, or maybe even some big misconceptions or myths surrounding the breast cancer screening or the mammogram itself?
Dr. Tello-Sjkerseth: Sure. So another question we get is: “I’m seventy years old, should I still be getting mammograms? How long should I get mammograms? At what age should I stop getting mammograms?” And that’s another controversial topic out there. And the vast majority of these different societies that come out with guidelines are saying it should be up to the patient and the provider together. So you can have that conversation with your doctor and decide at what age you might want to stop. Let’s say you’re 80 years-old. You could be perfectly healthy and maybe you’ll live 20 more years. So you’re probably gonna want to keep getting your, however, if you’re 80 years old and maybe very, very sick and have lots of other illnesses, and you may have a shorter life expectancy, maybe you’ll only be alive for another three or five years, or it may be, if you had got a cancer diagnosis at that age, you wouldn’t want to do any treatment. Anyway, you would just say, it’s, it’s fine. I’ll I’m, I’m at end of life. It’s okay. I don’t want to treat the breast cancer. It’s very specific to the woman. Most of these societies will say you should keep getting a mammogram until you have, um, less than a 10 year life expectancy. So you could be a healthy 80 year-old or an unhealthy 80 year-old and decide if you want to do mammograms or not. We do mammogram screening on 90 year-old’s. I’ve had one that was 100 years-old this year. So you can be very healthy and still be a pretty advanced age.
Host: What about men?
Dr. Tello-Sjkerseth: Men absolutely can and do get breast cancer. But it’s on a very smaller scale than women meaning the risk. I think of a man getting breast cancer is less than 1%. It’s very, very low, obviously much more common in women due to multiple factors, but yes, men can still get breast cancer. The men that do get breast cancer usually have some kind of family history of breast cancer or some other types of cancers that run in the family and they may have a gene mutation. Now we don’t regularly screen men for breast cancer. So they’re not getting mammograms every year for us to find them because the incidence is so, so low. So most of these breast cancer we find in men are the men that come in with a lump or some kind of abnormality on the skin that they’re noticing. And that’s how we find them.
Host: Okay, good to know. Let’s shift now to the COVID-19 pandemic and what impact COVID-19 has had on mammography at Sanford Health.
Dr. Tello-Sjkerseth: Breast cancer screening, specifically a modified did drop pretty significantly during those first few months specifically, you know, March and April, it started to come back a little bit in may. And a lot of that was, you know, patients just didn’t want to leave their homes. And, you know, some healthcare facilities were telling patients, you know, don’t come in unless it’s, you know, like an, excuse me, an emergency or some kind of actual problem. And in the grand scheme of things, it probably is okay to delay your screening mammogram maybe for a couple of months. But on the flip side of that, we also had patients that had a breast problem. They had a lump or they had discharged or pain, something abnormal. And those women waited months to come in to get evaluated. And unfortunately, we saw a lot of cancers in women that probably could have been found a lot earlier, but they waited a lot of these patients had issues in January or February and then just delayed it and didn’t come in until July, August, even this month. And we’re, we’re seeing them, these cancers being more aggressive cause we didn’t catch them earlier. Now, I will say we had some various women that still came in for their screening mammograms during the whole COVID time, especially that early time, because they were high-risk and they recognize the importance of getting their mammogram no matter what. And I know of three patients that were high risk that came in during their regular screening time and we found cancer in them. And if they would have delayed a few more months who knows how bad it could have been at that time, because those, those high risk patients usually have more aggressive forms of cancer.
Host: Emphasize again the importance of this screening and especially in a pandemic year that we’re in why it’s not okay to continue putting off this type of care and really encouraging women to get that screening done.
Dr. Tello-Sjkerseth: Yes. So as we said, breast cancer is the most common cancer diagnosed in women. One in eight women will get breast cancer in their lifetime and of those cancers, one in six will be in women in their 40s. Mammography is the gold standard for breast cancer screening detection. It is the only modality we have that has decades and decades of research supporting its use and its mortality reduction benefits. Meaning if you get screened every year, you go through the mammographic screening process, it decreases your risk of dying from breast cancer. That’s why it’s so important every year to get this done.
Host: As we wrap up, tell us how a woman might schedule her mammogram, or maybe just find more information about mammography at Sanford health.
Dr. Tello-Sjkerseth: We have a very active website at Sanford that describes mammograms and MRIs and breast ultrasound and high-risk screening. And what does high-risk even mean? It’s part of our Edith Sanford Breast Center website. We have something here called self-referral so you, anyone can essentially schedule their own mammogram. You don’t necessarily have to go through your doctor or other provider. You can schedule it yourself online, or you can call the radiology department any place you want and get it done. Now you don’t necessarily have to have your doctor at Sanford to get your mammogram here. We can send your mammogram report to any physician or provider you want. And same vice-versa. If you’re out of town or at a different facility, want to get your mammogram there, you can still do that and then get the results sent to your provider at Sanford. It’s very easy to schedule yourself. If you have a primary care provider, the order will go under that physician or nurse practitioner, whoever you see. If you don’t have someone that you can send your results to you haven’t, you don’t have a regular doctor. That’s okay too. You can still schedule your screening mammogram. And we have protocols in place that will assign a doctor to you who will get those results just in case you need to have more and more tests done, or someone to go over the results with you. And then you can choose whether or not you want to keep that provider, but there is always someone that can answer your questions and that will get your results. So they don’t just go off into the wind and you know, you’re left on your own, not knowing what to do,
Host: Dr. Tello-Skjerseth, really great information, insight and expertise. Thank you so much for joining us for this episode of One in Eight. A pleasure getting to talk to you. Thanks again.
Dr. Tello-Sjkerseth: Thank you so much for having me. I hope this helps.
…
Posted In Cancer, Cancer Screenings, Cancer Treatments, Imaging, Menopause Care, Physicians and APPs, Specialty Care, Women's