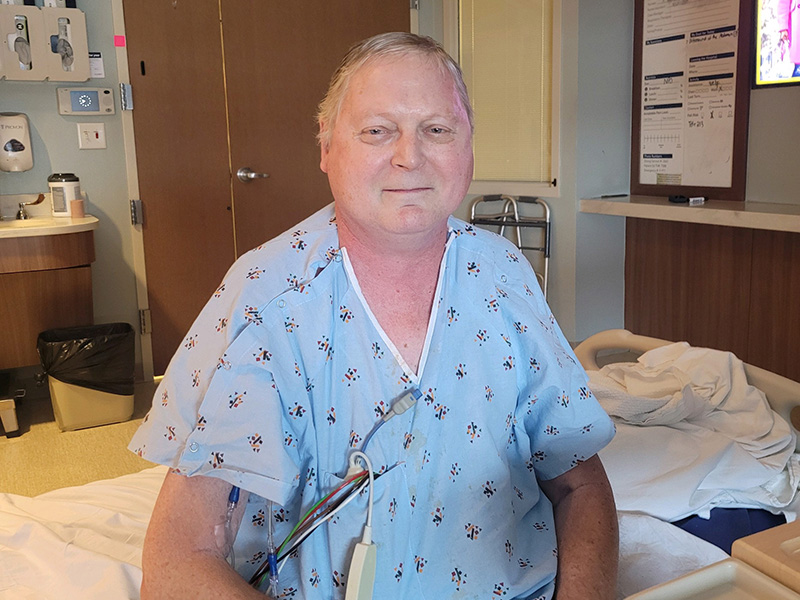
Darryle Hogfoss had his morning routine down pat. Every day started with him and his wife Jan taking a long walk.
“Usually we would get up right around seven to eight o’clock. And we normally had a route that we would walk and that ranged anywhere from two and a half to three miles, depending upon how hot it was that morning,” Hogfoss said.
Last April he started slowing down. At first he thought it was the flu until he started sleeping almost 22 hours per day. He couldn’t eat and lost roughly 40 pounds. Then his peripheral vision went away.
“All I could see was straight ahead. There was something going on,” Hogfoss said. “I went in to see my primary doctor. He took one look at me and said, ‘You’re a very sick man.’”
Diagnosing the pituitary problem
As his primary doctor, Stipe Ivancic, M.D. ran preliminary tests on Hogfoss, then referred him to Sanford endocrinologist Raul Ruiz, M.D.
“I was able to see that there were some abnormalities in the size of his pituitary gland,” said Dr. Ruiz. “That, along with all of the other symptoms, kind of started making sense that his hormones were shutting down.”
The pituitary gland is pea-sized and attached at the base of the brain. That little gland is in charge of an incredible amount of functions though.
“It controls the thyroid gland, it controls the adrenal glands, it controls ovaries and testosterone,” said Dr. Ruiz. “And then those other glands make hormones that practically work on every organ of our body.”
Hogfoss’ life was in danger.
“I was told by two physicians that I’m lucky to be here. That I almost died,” Hogfoss said. “At the time, I didn’t realize it, but looking back I can see that.”
MRI images showed the pituitary gland became much thicker than normal, so inflamed that it pushed up on the nearby optic nerve.
Most importantly in his case, said Dr. Ruiz, Hogfoss’ body wasn’t making enough cortisol. That’s a vital hormone that helps to maintain blood pressure.
“So the person then becomes very weak, cannot fight off any infections or inflammation. That is probably the most important and crucial (hormone) to replace right away, because that is when a person may die if it’s not done in time,” said Dr. Ruiz.
New normal
Hogfoss was treated at Sanford Health, and is now on hormone replacement, which he’ll need to continue for the rest of his life. He takes 15 pills a day, but he is on the mend. Even if his old routine looks slightly different now.
“When I do yard work, I bring out a chair. When I’m exhausted, I sit down and take a break,” he said. “I probably walk about a third of what I used to.”
He says the experience has given him a new, positive perspective as well.
“Things that weren’t quite so important are important to me now,” Hogfoss said. “When I travel, I look at the scenery. I used to look just straight ahead. Now I appreciate everything that is around me and the people that are around me. It’s a blessing.”
Learn more
- Juvenile diabetes diagnosis comes after medical scare
- High blood pressure is more serious than you may think
- Disorders of the pituitary gland
…
Posted In Endocrinology, Fargo, Internal Medicine