Sanford Health’s first-of-its-kind clinical trial using a patient’s own stem cells to treat shoulder injuries positions it to be a leader in the use of regenerative cell therapy to help people suffering from osteoarthritis and other more complex ailments.
“Sanford Health is a pioneer in this area, and this is the tip of the iceberg,” said Katie Pohlson, senior director of innovation and commercialization.
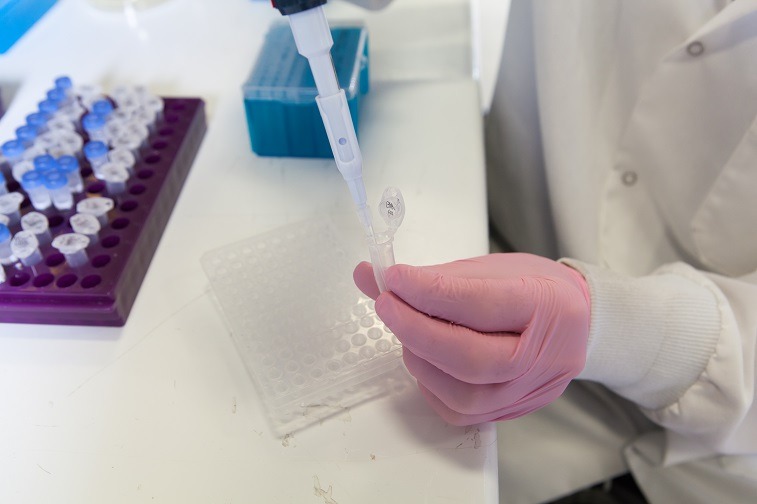
Cell therapy, a type of regenerative medicine, involves extracting regenerative cells from a patient, isolating them and injecting the cells into the same patient to repair and regrow tissue damaged by injury or disease. Regenerative cells include stem cells and several other cell types that work collectively to promote healing and repair damaged tissue.
In December 2016, Sanford Health physicians and scientists with partner InGeneron Inc. were the first to work with the U.S. Food and Drug Administration on a trial using adipose-derived stem cells in rotator cuff tears, the most common type of shoulder injury.
Because of the safety and success of that initial trial, the FDA approved a Phase 2 pivotal trial in 2019 involving up to 15 sites and as many as 246 patients. Like the first trial, the second study, which is currently enrolling patients, was sponsored by InGeneron.
The Houston-based company created a processing unit that separates stem cells and other regenerative cells from blood vessel walls in fat tissue taken from one part of the body that are injected into an area of disease or injury, said Christopher Alt, M.D., director of scientific and medical affairs.
“InGeneron’s cell therapy platform allows physicians to access the regenerative cell population in a patient’s own adipose tissue and redistribute those regenerative cells from an area where they’re in abundance to an area where they have been depleted and the natural healing capabilities of this tissue are no longer available or sufficient to maintain function,” he said.
Collaboration makes study unique
The first trial fell under the FDA’s early feasibility, or proof-of-concept, study. That program ensures patient safety while testing innovative technology on a small group before applying it to a larger population.
Sanford Health focuses on adipose-derived regenerative cells taken from the abdomen because they are plentiful and can be quickly and easily collected and then used in many parts of the body. The blood vessels in adipose (fatty) tissue also yield many times more stem cells than other sources, which can be returned to the body within hours and have a low infection rate.
“It was really a demonstration of a health institution implementing a very complicated study and introducing a lot of science into what could be deemed as a normal clinical application,” said Tiffany Facile, director of clinical regenerative medicine at Sanford Health, who helped initiate the trial.
“We collaborated with radiology. We collaborated with plastic surgeons, scientists, orthopedic surgeons, you name it, to contribute to this study and operationalize it. And at that time, it was unannounced in the nation about how to do this and how to do it the right way and how to keep it safe for patients. That clinical trial has led to a larger clinical trial, more sites, more patients. That’s really the pathway for clinical approval, is larger clinical trials, treating more patients, getting more data out there to the FDA to show how it works.”
Sanford Health orthopedic surgeon Mark Lundeen, M.D., in Fargo, North Dakota, was one of the principal investigators. They chose partial-thickness rotator cuff tears because patients have pain, may suffer from function issues and there’s no treatment option other than steroid injections and sometimes therapy in the hopes it repairs itself, Facile said. If it becomes a full tear, the person usually needs surgery.
How cell therapy works
If disease or injury inflicts an area of the body, its natural response is to produce an inflammation that regenerates tissue, which also causes pain, Dr. Alt said.
When a person’s own adipose-derived stem cells are injected into that area, the cells “take clues from their microenvironment,” recognize what part of the body they’re in and determine what they need to do to replace those dead or damaged cells, he said. “They adapt to the environment.”
Dr. Alt likens those cells to a newborn baby who can’t immediately do anything but has the capability to learn from parents, teachers and college professors and over time develop a specific set of skills that eventually makes them an expert in their chosen profession.
“With the cells, it’s very similar. These cells start out with all the capabilities but no function. They cannot do anything. They will then go on to develop into cells that are on the way, like an adolescent, and ultimately develop into experts which are then cells that have a specific function,” he said.
The cells show promise to regenerate damaged tissue leading to improved function and long-term pain relief, which means the person doesn’t need medication that might lead to an addiction to pain killers, Dr. Alt said.
‘Safest for patients’
Besides that societal benefit and the scientific innovation, which the FDA has recognized, Sanford Health is unique because it follows the rules in the use of stem cells, Facile said. As a nonprofit health care organization, its goal is to help patients.
“We tell patients exactly what the science shows. We tell patients exactly what they may or might not get for outcomes. We’re very open and honest with patients,” Facile said. “We know patients want to feel better. It’s hard to hear people tell stories about how they were charged a lot of money for “stem cell” treatments that treat using a questionable product.”
Sanford Health tests everything to ensure treatments have the right concentration and are free of bacteria, collects data and follows FDA rules and regulations.
“We have to do what’s safest for patients,” Facile said.
Treating other conditions
Sanford Health researchers have learned much about regenerative medicine in the rotator cuff trials and are using that knowledge to treat more complex ailments.
“We needed to start with that easy application first (shoulder tears) and then go to a larger population,” Facile said.
Patients from as far away as Florida, California and Hawaii now come to Sioux Falls for treatment in Sanford Health’s new orthobiologics program that offers adipose-derived stem cell treatments for osteoarthritis in five joints: hip, knee, wrist, ankle and shoulder.
Based on those outcomes, treating patients with rheumatoid arthritis and other conditions might also be possible, Pohlson added.
“I think one of the great things about InGeneron is it’s a platform technology. So currently the primary indication they’re going for is for partial rotator cuff tears. But there’s the possibility of going for a knee indication or even other types of indications like cardiac or different neuro disorders. There are endless possibilities with this technology,” she said.
Sanford Health also utilizes other orthobiologic technologies to pull therapeutic cells from bone marrow and treat people with tennis elbow or a shoulder tendon tear.
“One of the keys to Sanford partnering with companies like InGeneron is we’re able to bring these innovative technologies into Sanford to benefit our patients. And we’re also a large, integrated health care system” that supports its partners, from smaller startups to more established companies like InGeneron, Pohlson said.
“We’re able to give them some resources and work with them to help them advance their technology and get into the clinical environment.”
…
Posted In Innovations, News, Research