I’ve always been a planner. I like to anticipate, prepare — or brace – for the many situations that could be encountered in life, in a day, or even just on an errand.
And then I learned 10 years ago that I was pregnant for the first time – with twins. At the “old age” of 35, no less. The internet will happily tell you all about the risks that abound with pregnancies that involve multiples, or with that dreaded phrase “advanced maternal age.” It rubs its palms together in eagerness to frighten would-be moms with phrases such as “preterm labor.”
Expecting fraternal twins, I certainly had plenty to plan for. But even given my general good health, so much was out of my control. I could eat, but I couldn’t necessarily make the babies grow; my main goal was to carry them as long as I could, knowing twins usually deliver early.
I could also make sure we had diapers and other newborn necessities ready, but I couldn’t give them a nursery apart from sharing the master bedroom with my husband and me yet. (Because of a basement-finishing-project-in-progress, their future main-floor bedroom remained a storage room full of stuff until they were at least 9 months old).
And I could buy a breast pump and specially sized Boppy-type pillow for nursing twins, but I couldn’t guarantee that any of us would get the hang of breastfeeding.
Signs pointed to a C-section
Looking back, I realize at this time in my life, I surrendered the belief that I could plan for everything. I’d like to say I never worried about outcomes again, and I’ve been perfectly at peace since then, but … I would be lying. Especially since I’ve been raising twins. However, it does seem to get easier to recognize the times I do get out of balance.
So I went through pregnancy focused on growing two babies: making it to all of my Sanford Health ultrasound and prenatal visits; attending childbirth classes; diligently counting Braxton Hicks contractions to be sure I was not, indeed, in preterm labor; and in the meantime, helping install and finish drywall on our basement project. The last was definitely the least fun part of pregnancy for me.
I think all of the uncertainty involved in a twin pregnancy sort of distracted me from setting up a lot of expectations about what delivering and having infants would be like. Beyond a lot of diaper changing, feeding and burping, of course. As I sat through the childbirth classes at Sanford Health, I thought all of the options for labor (birthing ball, whirlpool, etc.) sounded really cool, but I assumed I’d end up with a C-section. That’s more common with twin deliveries to begin with, and my twins were transverse every time I had an ultrasound (lying sideways, one on top of the other, with the foot of Baby B on top treating Baby A’s head like a soccer ball).
Suddenly, I was cramming for labor
Then suddenly I got to about 35 and a half weeks along, dilated a centimeter or two, and an ultrasound showed that Baby A had moved head-down, ready for a vaginal delivery.
Thought No. 1: How did I not notice two babies that far along had completely switched themselves around? After all, I felt every punch to my bladder and every time a spine or skull seemed to bruise my lungs and ribs, but somehow I completely missed the big “moving day.”
Thought No. 2, following closely behind: I wasn’t paying enough attention to the vaginal delivery part of my childbirth classes. Now, I basically had to cram like it’s college finals week. How does the breathing go again? How long could it take to dilate to 10 cm?
I was glad that I, right away, had dug out and pored over my childbirth class “manual” when, two days later, real contractions started in the middle of the night, and my water broke. Liquid gushing with every contraction, I completed packing my partially filled duffel bag, called the hospital and got my husband going. I figured we’d have plenty of time, first delivery and all. I swear that’s what my childbirth classes promised.
Step on it!
We got into the car about an hour or so after I’d awakened and started heading out of our bedroom community to Sanford USD Medical Center’s emergency department. We made it about eight blocks. And then a sheriff’s deputy, probably bored on his small town assignment at 3 a.m. on a Wednesday, found something to do: stop a sedan suspiciously exceeding the speed limit in our 25 mph zone through town.
My husband was in no danger of actually receiving a speeding ticket once he pointed out his ultra-pregnant-looking wife in the passenger seat (my stomach had measured 44 weeks at my last appointment). We did keep the deputy busy escorting us to Sioux Falls, however.
In the Sanford USD Medical Center emergency department, they checked to see how dilated I was. And then things became more urgent: I was at 8 cm and still had to make it to The Birth Place.
I have a vague memory of riding in a wheelchair through hallways and an elevator, and then I was in a labor room but told not to get too comfy. With twins pending and a C-section still a possibility, I would head to an operating room after the OB-GYN on call arrived and “suited up.” In that labor room, we discovered I’d dilated to 10 cm already.
Hurry up and wait
I felt fortunate the pain hadn’t been excruciating up to that point, and I really didn’t have a strong opinion about whether I wanted pain medication. But when the doctor asked me, as she scrambled into scrubs, if I thought I could stay relaxed if she had to reach up and maneuver the second baby after the first was born, I decided that didn’t sound relaxing at all. So an anesthetist swiftly injected spinal anesthesia, and I was whisked into the operating room.
With the pace of everything up to that point, you’d expect to hear I pushed once or twice and delivered the first baby 10 minutes later, right? I was surrounded by what seemed like a robust team of people, from nurses to the doctor to neonatal teams, plus my husband, all vigilant for that moment.
But then things slowed way down. I pushed when the nurses told me to, though because of the anesthesia I couldn’t tell for sure whether I was doing it “right.” I assumed I was doing OK because nobody said to do anything differently, but each time the baby did not come out, so I just kept pushing on command. I kind of felt like a kid myself, when you don’t completely know what’s going on in a situation, so you just follow along pleasantly, dutifully, and wait for whatever comes next.
Our first meeting
So apparently, the problem was the first baby’s head – not quite lined up right, it refused to emerge. Eventually, to avoid tiring me out before I had a second baby to deliver, the doctor used a vacuum to assist with Baby A. I didn’t think I felt that tired, but I also didn’t know if the baby would be stuck there all day. Ultimately, I was happy to bow to the wisdom of the professionals.
So, the first baby girl came out just fine, and a neonatal team finally had something to do. I couldn’t really savor the moment, though, because it was time to focus on the second one.
Then the pace picked up again – the doctor discovered her heart rate was dropping in utero, so Baby B came out quick with a vacuum as well. Her neonatal team had more to do – she wasn’t breathing right away, but she was in great hands that rapidly restored her to living, breathing life.
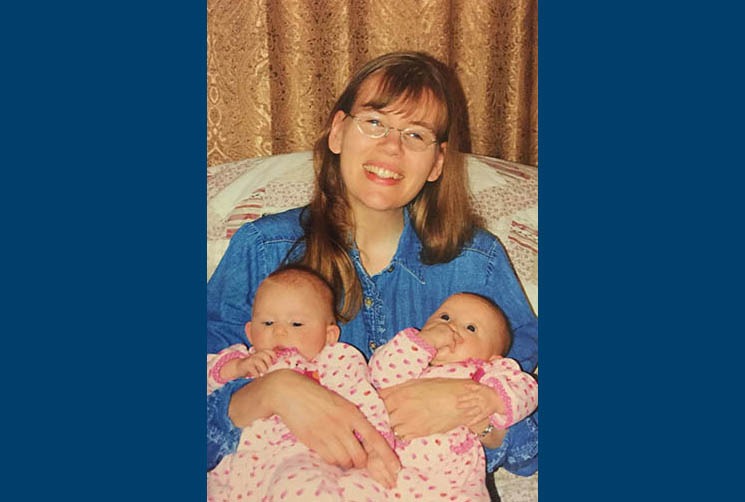
And then suddenly I was holding two swaddled girls, one less than 5 pounds, one a little over 5 pounds. No planning can quite prepare you for the moment when you get to look at the faces of your brand-new babies for the first time, either.
More stories
- Making your birth experience the best it can be
- It’s twins: Prenatal care for multiples
- Labor nurses bring calm to storm of new motherhood
…
Posted In Children's, Gynecology, Pregnancy, Sanford Stories, Women's