Sanford Health began addressing concerns involving Nick and Jill Jay’s son Max when he was still in the womb. In the five years since then, no one has given up on fixing the clubfoot he was born with, or the associated complexities that have come his way.
At Jill’s 20-week ultrasound visit at Sanford Maternal-Fetal Medicine in 2020, a possible problem with their son’s foot was detected. When this was later confirmed, it set in motion the beginning of an ongoing treatment plan that remains focused on improving his outcome.
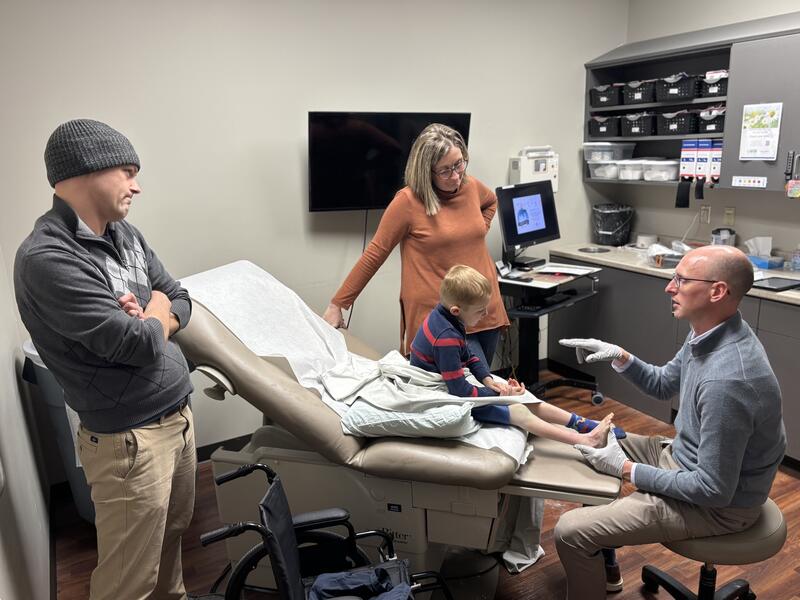
When Max was two weeks old, Nick and Jill, who live in Cottonwood, Minnesota, had a meeting with Jared Daniel, M.D., a Sanford pediatric orthopedic surgeon in Sioux Falls, South Dakota. He explained they were going to improve the position of the foot and allow their son to walk with a flat foot as he grew older.
Max’s care has followed a conventional path in many ways but also involves elements of ingenuity and a memorable level of attention to the family’s needs.
In an email Jill sent to Sanford Health, she related the following about Dr. Daniel, and Rob Safar, the certified nurse practitioner who was also part of Max’s most recent surgery:
“We are so blessed to be able to have Max see Dr. Daniel and Rob and will continue with them in the future,” she wrote. “We just want you all to know that finding providers like this is very hard to find. They have blessed us beyond measures and shown on God’s working mercies.”
Clubfoot basics
To get a better idea of what Max and his family have been up against, it’s best to know some of the fundamentals about treating a child born with this congenital defect.
Like other parents who have babies with clubfoot, the Jays got to know their son’s providers very well. Clubfoot can successfully be treated, often with dramatic improvement, but it takes time and lots of doctor visits.
“A beauty behind clubfoot treatment is that we get to see the families many times before we do something,” Dr. Daniel said. “The history of doing casting on a weekly basics for five or six weeks, then seeing them for follow-ups over the next several years – two or three times a year – establishes a rapport.”
Doctors treat clubfoot with the Ponseti Method. It involves stretching the baby’s foot with a corrective cast that is reapplied weekly for several weeks. Many babies then need a small procedure to release the tight Achilles tendon, followed by wearing special boots that are braced against the other foot. This brace is often referred to as “boots and bar” and helps keep the feet pointed outward.
The brace is worn pretty much all the time initially for the first three months and eventually only while sleeping. The process takes several years.
“We talked with Dr. Daniel about what we would be doing moving forward,” Jill said, recalling their first meeting. “We knew at that point that this was going to be a journey. There are a lot of times as a parent you go in and you want answers and you want to fix it, but this was going to be a journey we were looking at that might last the rest of his life.”

Photo courtesy of the Jay family
Treatment obstacles
Max, the youngest of the Jays’ four kids, is an energetic child who has often found ways to explore the outermost boundaries of his care plan, especially when he got a little older. His resilience, though a bit of a task at times, has been heartening to see.
At 9 months, three toes on Max’s affected foot began to curl under. A procedure with Dr. Daniel released the tendons and allowed his toes to lay flat again. At 18 months, he was walking and doing his best with the boots-and-bar presence in his life.
When he was 4, they began the transition from the “boots and bar” Ponseti Method to what they hoped would be normal mobility. There were early signs, however, that he would need an additional procedure.
“It seemed like he was having what we call ‘dynamic supination’ where when he walked, he had the tendency to want to turn his foot in and walk on the lateral border,” Dr. Daniel said.
The procedure used to address this issue is a tendon transfer that rebalances the foot. This surgery involves taking a tendon located on the inside of the foot and reattaching it to the outside. The result is that the foot stays straighter.
During the procedure, however, Dr. Daniel discovered another problem: The tibialis anterior tendon that he was going to transfer was connected to the muscle right next to it, known as the extensor hallucis longus.
Dr. Daniel called it a rare “anatomic variation,” and it meant the surgery he had planned to execute was not going to work. Instead, he opted for a “split transfer.” It involves a longer, more intricate incision but would still allow them to harvest the anterior tendon and safely move it over to the lateral side of the foot.
Waiting patiently
While this was going on, the Jays were waiting to hear the surgery was over. Jill, a nursing manager in Minnesota, understood this procedure was going to take about an hour-and-a-half. When that time window came and went, she got a little anxious. Was there an issue? Why was this taking so long?
The staff offered to tell Dr. Daniel that she was curious about the delay. Jill said no to that, however. Best to let them do their jobs.
“I decided I wanted Dr. Daniel and Rob to just focus on my child and not worry about a mother’s brain and what rabbit hole I’m going down right now,” she said, laughing. “I just needed about 15 minutes outside to get some fresh air.”
When she returned, they were almost done. A little later, Dr. Daniel appeared and told them why it had taken so long and how they solved the problem.
“I was thinking that a surgeon could just close him up and be like, ‘Oh, well, there’s nothing else we can do. He had this additional anomaly,’” Jill said. “But Dr. Daniel is so caring that he was like, ‘No, we have to think on our toes and come up with the best outcome for Max.’”
Dr. Daniel had never before dealt with a clubfoot patient who had those tendons fused together. He had used the split tendon technique for other kinds of procedures, however. He was also as knowledgeable as a human could be about Max’s foot, having first seen it when the boy was two weeks old.
That helped explain why his decision to move forward with a different script, while unconventional, was based on previous groundwork.
“At the time of the procedure it was a challenging decision point,” Dr. Daniel said. “But using those fundamentals – and the knowledge that you go through with all that training all those years ago – helps you out.”
Care from the beginning
The information needed to make decisions on Max’s care began arriving at the 20-week ultrasound four months before he was born. It serves as an example of the value of prenatal care for babies and their parents, as well as the emphasis placed on it at Sanford Health.
Shelby Ellwein is an RN who is the Sanford Fetal Care Coordinator. She keeps a running list of patients who have a special prenatal prognosis and may need specialty care when they’re born. As was the case with the Jays and their son Max, it can give parents a head start on planning for their baby.
For the Jays, this meant understanding Max would be part of a care plan that would include boots and braces and patience. For the Jays, that meant they were prepared for the possibility their son would be born with a clubfoot. It meant two weeks after he was born, they were already talking with a pediatric orthopedic surgeon about how they were going to take this on.
“Having a baby is enough of a surprise and enough excitement all on its own,” Ellwein said. “So knowing some of these challenges or just unexpected things ahead of time gives them time to wrap their brain around it and understand what they’ll need to care for their baby.”
For the Jays that meant understanding Max would be part of a care plan that would include boots and braces and patience. The underlying philosophy applies to all parents getting ready to have a baby.
“Once we have a diagnosis, we get all the important smart people in the room who can make the best plan for that baby,” Ellwein said. “On the patient side of things, I’m the contact. I help coordinate their prenatal appointments with whatever specialties apply, whether it’s pediatric cardiology, pediatric surgery, pediatric nephrology – whoever it might be – and we get those appointments arranged for a time that works for them.”
Ellwein’s work can provide reassurance at what is often a stressful time. While connecting a patient and a diagnosis with all the “smart people,” she is helping families reach a level of peace they might not enjoy otherwise.
Something more
The Jays have been witnesses to Dr. Daniel adding acts of kindness to the clinical care package he provides the parents of young children in a time of need. Preceding Max’s most recent surgery, Dr. Daniel made sure the Jays got a wheelchair for Max a week before he would be in a cast. He wanted Max to get the hang of a wheelchair before he actually had to use it.
Then there was the night before the surgery. Dr. Daniel called to tell them their son’s surgery was going to be delayed a few hours while he and Rob Safar delivered care to another patient.
A minor detail, given the circumstances? Perhaps. But the Jays would be traveling more than 100 miles from their home in Cottonwood to Sioux Falls and they had planned to leave at 5:30 in the morning.
“He said, ‘Why don’t you come in like two or three hours later so you don’t have to sit in the waiting room with a 4-year-old who is going to be jumping all over the place?’” Jill said. “I’m like, ‘OK, why are you, the surgeon, calling me and telling me this?’ But that’s just who he is.”
Within two hours of the surgery to move his tendon, Max was wiggling his toes.
“We count that as a win and a blessing,” Jill wrote in her email. “These two providers have far surpassed what they needed to do.”
Learn more
- Prosthetic helps young patient after leg amputation
- After life-changing UTV crash, teen commits to recovery
- Jackrabbit junior completes cheer comeback after amputation
…
Posted In Children's, Orthopedics, Pregnancy, Sioux Falls, Specialty Care, Women's