You’re a woman in your 20s, excited about your upcoming wedding. You’re heading to your bachelorette party with close friends, but on the way you have to find a gas station restroom — now. It’s that all-too-familiar urgency that won’t leave you alone, even for a special evening.
You’re a man in your 30s, training for a marathon. You’re working up to running 40 or 50 miles a week, but you’re also forced to plan runs around bathroom breaks to avoid an accident. Is the exhaustion more from the training? Or from the constant loss of blood?
People with Crohn’s disease or ulcerative colitis symptoms tend to think about bathrooms a lot: Where’s the closest one? How loose will the next bowel movement be? Will there be blood?
Inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, affects more than 3 million people in the U.S., according to the U.S. Department of Health and Human Services. But while it can be a significant factor in their lives — for the rest of their lives — treatments personalized for their unique case can make a big difference.
‘I put it off for too long’
Retta Hausman is that woman who had to stop for a restroom break on the way to her bachelorette party. But that’s almost a lighthearted view of Crohn’s disease compared to what it put her through just two weeks before her wedding in the summer of 2016.
Hausman had struggled for more than two years by then with unrelenting, uncontrolled inflammatory bowel disease.
She’d first started having bloody diarrhea in January 2014, but she hesitated and didn’t see a doctor until that August.
“I was unsure of what it was. I was nervous,” Hausman remembered.
“One of the reasons why I didn’t go in soon enough was that I was really embarrassed to talk about it. I put it off for too long.”
In August, she saw a specialist at the Sanford Center for Digestive Health. There, a colonoscopy led to her initial diagnosis of ulcerative colitis, which is typically an inflammation of the colon in the gastrointestinal tract.
Finding out that she had a lifelong disease, in her 20s and looking forward to forming a family, was a shock.
“It’s a lot to take in at first. I didn’t really know what it was or how it was going to affect me,” Hausman said.
But she learned. “It affects you every day of your life for the rest of your life, because there is no cure,” she said.
The bond between patient and doctor
Even with a diagnosis and medications, however, nothing seemed able to get Hausman’s disease under control. It wasn’t through lack of trying — a bond had formed between Hausman and her Sanford Health gastroenterologist, Brett Baloun.
In the process of treating patients for a lifelong condition, and exploring options with them, doctors can become more like friends.
“He’s easy to talk to,” Hausman said about Dr. Baloun. “You can really tell that he cares about his patients.”
Dr. Baloun considers his relationship with patients, who entrust their health and lives to him, an “absolutely rewarding” part of his job.
“I get the opportunity to work with truly wonderful, great people like Retta,” he said. “To be involved in their lives to the extent we are, it’s really an honor. In the end it’s those connections that make this career completely worth it.”
"The disease was really taking over." Retta Hausman, patient at Sanford Center for Digestive Health
In the summer of 2016, Hausman relied heavily on her connection with Dr. Baloun and his calls to check in on her. She had her wedding to look forward to, with all the planning and excitement that this momentous event entails. But her medical issues were becoming severe. She had extreme abdominal pain, along with diarrhea up to 15 times a day.
“I wasn’t able to leave my house much,” except for work, Hausman said. “Anywhere I went, I had to know where the closest bathroom was.
“It was a really difficult time in my life because the disease was really taking over.”
‘Do we need to postpone the wedding?’
The available treatments weren’t working well for Hausman, including high doses of short-term steroids intended to relieve severe symptoms. Dr. Baloun has built relationships while working with Mayo Clinic providers, so he decided to refer her to a gastroenterologist at Mayo who specializes in inflammatory bowel disease.
By the time Hausman arrived for her appointment at Mayo, shortly before her wedding date, she was so sick that doctors admitted her to the hospital. First, they focused on a Clostridium difficile (or C. diff) infection they discovered, a contagious bacterial infection that can cause diarrhea and inflammation of the colon, among other symptoms. Having IBD can make a patient more susceptible to a C. diff infection.
Hausman received treatment in the hospital for C. diff for five days. During that time, doctors discussed with her which treatment option for IBD would best help her feel well and healthy enough for her wedding in two weeks.
“I just remember being in the hospital room with my future mother-in-law, and we were talking: Do we need to postpone the wedding? Am I going to make it through? Am I going to be healthy enough?” Hausman said.
Surgery, then a wedding, then a move
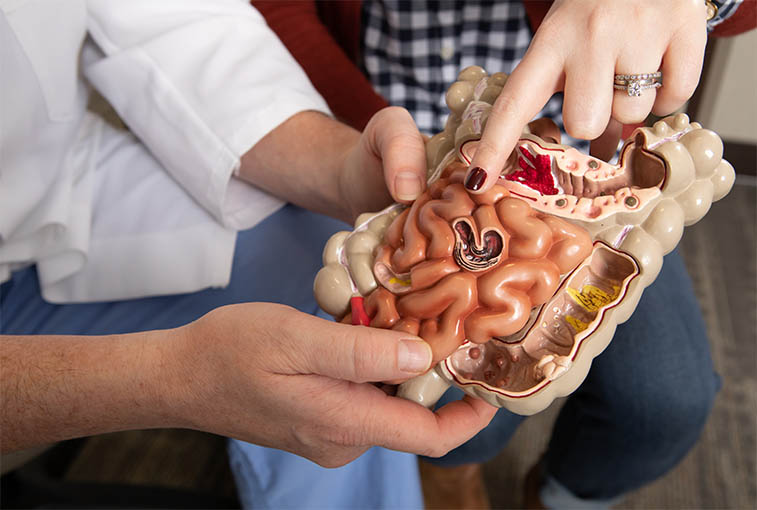
Ultimately, the Mayo doctors decided with Hausman that the best way to relieve her symptoms quickly and give her colon a chance to rest and heal would be an ileostomy surgery while she was there. “A little bit of a bypass,” as Dr. Baloun puts it, the temporary ileostomy closed off her colon and brought a loop of bowel through an opening, or stoma, on her abdomen. This way, solid waste would exit her body through the stoma into an external pouch rather than 15 times a day via her colon.
Meanwhile, the doctors also debated whether Hausman had ulcerative colitis, or whether she actually had Crohn’s disease. While symptoms may be similar, Crohn’s disease can involve any part of the digestive tract — not just the colon — from the mouth to the anus.
In communicating with Dr. Baloun about Hausman’s previous medical history, Mayo doctors concluded she actually had Crohn’s disease. A procedure at Sanford Health had spotted granulomas in her stomach, though oddly not in her colon, where her problems were occurring. Granulomas, or small masses of inflamed tissue, may appear in Crohn’s patients but do not in ulcerative colitis patients.

Submitted photo
Hausman spent more than two weeks at Mayo, in that time recovering from a serious bacterial infection and going through serious surgery — but she arrived at her wedding as scheduled.
“I made it through the day,” Hausman said. “It was OK, but it was a little tough.”
Then the next day, she and her new husband moved into a house they had closed on the week before.
Between the stress of her illness, wedding and moving, “I lost almost all of the hair on my head,” Hausman said. “When your body goes through a major stress, it will protect your vital organs first, and then it will sometimes let other things that are not as important go. … I ended up wearing a wig for about a year until it grew back thicker and longer.”
Adapting to the ileostomy
Back home and under the care of Dr. Baloun, who still collaborates with Mayo about her care plan, Hausman started a new medication regimen and adapted her diet to her ileostomy.
With her colon on an extended vacation, her small intestine is not just responsible for doing its own job of digesting food. It also has taken over the colon’s job of absorbing water. Tasked with so much now, the small intestine may have trouble doing either job really well — something Hausman has noticed.
“Certain foods like nuts and seeds and some raw vegetables, they just don’t break down. So I do have to avoid those foods so I don’t get a blockage,” Hausman said.
“You basically have to chew the food until it’s like mush before you swallow,” she added.
It’s also easy to get dehydrated without a functioning colon. Hausman drinks a lot of water to help compensate, but she still has ended up in the hospital for dehydration. Some medications used to treat IBD can weaken the immune system as well, contributing to hospitalization.
Hausman spent time in the hospital twice last fall. One stay lasted five days, when she had C. diff, E. coli and norovirus infections all at the same time. The other stay was two days during a Thanksgiving trip to Denver, when she caught a virus and became dehydrated. So, like many people with weakened immune systems, she tries to avoid people who are sick, and she washes her hands frequently.
“You just get really tired of being sick all the time,” she said about the hospital stays. “You just feel like you can’t catch a break.”
‘I finally have the Crohn’s under control’
It took four years, but Hausman finally feels better now. “I feel like I finally have the Crohn’s under control,” she said. Doctors have found the right dosage for her medication regimen, which includes a Stelara injection every four weeks.
Now that her disease is more stable than it’s ever been, Hausman and her husband can pursue their dream of having children. They have visited a fertility specialist to make sure her previous abdominal surgeries — for appendicitis and the ileostomy, both laparoscopic — didn’t cause scar tissue to block her Fallopian tubes. Fortunately, the tubes were clear.
Eventually, after she’s finished bearing children, Hausman envisions having her colon removed completely, since her Crohn’s disease has been contained in her colon. Crohn’s could still show up elsewhere in her digestive tract, but Hausman anticipates a better quality of life with no ileostomy bag, less pain and more energy.

A case of uncontrolled ulcerative colitis
Brett Gaul is that man who trained for and ran a marathon despite a worsening ulcerative colitis condition.
With his initial diagnosis of ulcerative proctitis, which is inflammation limited to the rectum, earlier in 2016, he hadn’t been too alarmed. His symptoms included bloody bowel movements, rectal bleeding, abdominal pain and cramps, but he first figured they were just a hemorrhoid condition like he’d had in the past. When the symptoms didn’t go away, he visited a doctor for the diagnosis.
“Before these symptoms hit, I was a normal, healthy person. I was pretty active. I wasn’t on any medications,” Gaul said.
“But once these symptoms hit, it really did take away from my life. I wasn’t able to live the life that I wanted to live. I’d have to be careful about events and being close to a bathroom.”
The diagnosis ended up being ulcerative colitis after a colonoscopy looked closer. But Gaul thought he could just take medication and get back to his normal life.
“When I was sick before, I’d have to be really sick to go to the doctor, and I’d see a doctor, I’d get some medication, I’d get better, and that was it. So I thought this would be a similar thing. But it turned out that it was a much different thing.”
Training for marathon, ‘I just felt run down’
Initially, his medication in suppository form worked to relieve symptoms. But then it stopped being effective. Same thing with an oral medication he tried. And then it was early summer, with the marathon approaching at the end of summer. The frequent bloody stools were back — and getting worse.
“Obviously, training for a marathon is difficult. I was getting my way up to 40, 50 miles a week, and so you’re tired from that. I was also tired from dealing with these symptoms where I’ve got to time my bathroom breaks. I’ve got to go to the bathroom right before I go running. … I just felt run down. You know, I’m losing blood,” he said.
“I think at this time, too, I maybe started to cut back on what I was eating because my thinking was, well, if I eat less, I’ll have to go to the bathroom less, so that’ll solve the problem.”
“Of course, that just makes things worse, because I’m weaker, not getting the nutrients that I need while I’m doing all this intensive training. So that was obviously not a very good strategy.”
‘The race went well’ — but symptoms worsened
Gaul, now 42, of Marshall, Minnesota, had run marathons a couple of decades ago, but he wanted to improve on his time. He had done well running in more recent half-marathons, so he decided to train for the Sioux Falls Marathon, with the goal of a more competitive time.
“The day of the marathon, I felt good,” Gaul said. He felt as prepared as a person could be while dealing with his condition.
“But I did wake up that morning, and I did have a loose bowel movement, so I thought, ‘I need to be careful here because I don’t want to have an accident during the Sioux Falls Marathon. So I did take some anti-diarrheal pills that morning,” he said.
Enlarge
“The race went well. Like many people, I struggled once I got to about mile 18, and I hit the wall, as they say, so I slowed down. I didn’t finish as fast as I would have liked.” Nevertheless, Gaul finished with a personal record that was more than a half-hour under his previous time.
Once the September marathon was over, Gaul cut back on training and thought he would feel better — less tired. But his symptoms worsened further, and his first appointment with a specialist at Sanford Health, gastroenterologist Jorge Gilbert, wasn’t until November.
Gaul thought he could make it, but in October he was experiencing personal records of a different kind: bowel movements. They were increasing up to 10 a day, with 15 on one particular day. They were waking him during the night.
“You go to the bathroom. You go back to sleep. Two hours again, you’re awake again — you have to go to the bathroom. So it was challenging to get adequate sleep and basically just to live a life,” Gaul said.
‘This is much more serious than I ever thought’
The college philosophy professor and honors program director tried to keep disruptions at work to a minimum. “Fortunately, I was able to get in and out of the classroom to go to the bathroom when I had to. That only happened once where I thought, I could have trouble right here in the classroom,” Gaul said.
But while he was speaking with a nurse for Dr. Gilbert one day about his symptoms, she told him he needed to go to the hospital. “I knew I was in a bad way,” Gaul said, “but because it had really progressed so slowly, it wasn’t like there was one moment where I thought, ‘Wow, this is really serious. I need to get to the hospital.’ ”
Gaul’s hospital stay at Sanford USD Medical Center that October involved a colonoscopy that revealed how much more inflamed his colon had become.
Dr. Gilbert came to meet him for the first time. “I don’t think he’s much of a hugger, but I hugged him,” Gaul said. “I was so happy to see him.”
Dr. Gilbert explained how serious Gaul’s condition was: So far, his medications hadn’t worked, including a steroid that typically should relieve symptoms. And 70% to 80% of people in that position have to have their colon removed.
“Then I knew … this is much more serious than I ever thought it would be,” Gaul said.
Dr. Gilbert suggested Remicade infusions for Gaul. And finally, after two weeks on the new medication, Gaul could see hope for improvement. He gets infusions every eight weeks.
“I’ve been on Remicade for almost two years now, and now my life is basically like it was before. I feel back to normal,” Gaul said.
“I’ve been lucky where I haven’t had any flare-ups yet, so I consider myself in remission.”
The challenge with IBD isn’t just physical
Inflammatory bowel disease takes a toll. Physically, Hausman and Gaul both have struggled to just be well enough to work and live. Mentally, too, it can be a struggle to get up every day with a disease you know you’ll have for the rest of your life.
Hausman and Gaul have found support through their doctors and nursing staff, who take the time to listen and treat them like more than just the next patient on their schedule for the day.
Help also has come from their families, who so many times have been able to do nothing but watch their loved one get sick and exhausted and, at times, unable to participate in life.
Gaul has leaned on his wife and kids, as well as his mom, who is a retired nurse.
Hausman said of her husband, Nick, who takes her to the emergency room and sits with her in the hospital: “He basically is my caretaker when I was really sick, and he didn’t sign up for this.”
"It’s hard to watch somebody suffer and also try to be the person to help fix it, and it’s not immediate sometimes." Dr. Brett Baloun
Before his ulcerative colitis got under control, Gaul had to be hospitalized twice, for five days each. His students were concerned, so he ended up spelling out for them and his colleagues what was going on — why he hadn’t been in class, and why he might have to suddenly leave the classroom.
“There really wasn’t any way to sugarcoat it,” Gaul said. “I just said, ‘Look, here’s the issue,’ and they learned a lot about colon health that day that they might not have been anticipating.”
That transparency made him feel better — and he has discovered connections when talking with others about IBD. “I was surprised at how many people I knew had faced similar issues in the past,” he said.
Hausman has found it helpful to join groups on Facebook and hear other people’s stories there. For example, she’s in a group with people who take Stelara. “It’s interesting to read what other people are doing and how your treatment compares to theirs,” she said.
While patients can face steep mental challenges, doctors aren’t immune to them, either.
“When you’re not feeling well, I don’t feel good,” Dr. Baloun said of his patients. “It’s hard to watch somebody suffer and also try to be the person to help fix it, and it’s not immediate sometimes.”
‘Get the help that you need’
Her years of challenges have given Hausman time to reflect on what advice she might share with someone newly diagnosed with a chronic illness.
“There’s gonna be good days, and there’s gonna be bad days. But I think that if you have a strong support system and a team of doctors behind you, that’s going to make all the difference, and you are going to be OK,” she said.
Also, she added, “It’s really important to be an advocate for your health and to really do research behind the disease that you have and really understand it the best that you can.”
Gaul repeated several times his best advice for those trying to deal with symptoms but unwilling to talk about them: “Just be brave.”
“Let people know that this is happening with you so they can do the tests to find out what exactly is wrong with you, and so you can get the help that you need,” Gaul said. “Because the odds are, these symptoms aren’t going to go away on their own.”
And then he shared some advice Dr. Gilbert gave him. The doctor saw Gaul struggling with the notion that he has this lifelong condition. Gaul says Dr. Gilbert told him that wallowing in it doesn’t make it any better. “Just don’t think about it. Distract yourself. Do other things,” Dr. Gilbert told him.
As Hausman and Gaul have made it through the lowest points of their diseases, they’ve come to a place where this advice is easier to follow. Crohn’s disease and ulcerative colitis can now take a back seat to family life, work, hobbies — just where the diseases should have been all along.
"Let people know that this is happening with you so ... you can get the help that you need." Brett Gaul, patient at Sanford Center for Digestive Health
Symptoms, diagnosis and treatment
Crohn’s disease may affect any part of the digestive tract, while ulcerative colitis is focused mainly on the colon. But symptoms of Crohn’s disease and ulcerative colitis can be similar, including abdominal pain; loose, bloody stools; rectal bleeding; weight loss; fever; joint pain; rashes; fatigue; and eye conditions.
Both diseases tend to start in younger people, between the ages of 15 and 35, and affect both men and women. People with a family history of the diseases may be at higher risk.
A variety of tests may be used to diagnose the diseases and can include blood tests, stool cultures, colonoscopy, upper endoscopy (which looks at the upper part of the digestive tract), imaging and biopsy.
Treatments are tailored to each patient, but Dr. Baloun prefers to start out with less powerful medications that are very safe and have few side effects — “the first rung on the ladder” of treatment. If that doesn’t prove effective in controlling symptoms, he’ll move up a rung to something a little more powerful. As the power increases, though, so do potential side effects, which he discusses with patients.
Steroids, which can have an array of side effects as well, are short-term medications used to knock down severe symptoms. Longer-term medications are meant to keep symptoms at bay.
And surgery may be an option for some patients as well, such as removal of the colon.
Lower digestive tract diseases with similar symptoms
Irritable bowel disease may share some symptoms with other types of gastrointestinal diseases. A visit to a doctor and a variety of tests can help determine which disease a patient might have. Treatments vary for each as well. Here’s a brief look at some other diseases.
Irritable bowel syndrome: A chronic condition affecting the small intestine and large intestine. It may cause cramps, gas, bloating, diarrhea or constipation, and mucus in the stool. Women are at higher risk, and it often affects people before the age of 45.
Celiac disease: A chronic genetic condition in which gluten damages the small intestine and prevents it from taking in nutrients from food. It can cause symptoms such as chronic diarrhea or constipation, weight loss, gas, pale stools, anemia, osteoporosis, abdominal pain or bloating, joint pain and skin rash. It can appear at any age.
Diverticular disease: A group of chronic conditions in which tiny pouches form in the colon and bulge out through weak spots. These can range from no symptoms to pain or cramps in the abdomen, bloating and constipation. If the pouches get infected, signs of infection may appear such as fever, nausea, vomiting and chills. Males older than 50 are at higher risk.
Hemorrhoids: A condition when blood vessels in and around the anus and lower rectum become swollen and irritated. Symptoms can include blood in the stool; pain and irritation, swelling or a hard lump around the anus; and itching. Men and women may get this condition, including half of all people by age 50.
Colorectal cancer: Cancer that develops in the large intestine, usually as polyps, or growths, on the inner lining. Early cancer typically has no symptoms; later in the disease, symptoms may include rectal bleeding, abdominal cramps, weight loss, change in bowel habits and fatigue. Men and women may get colon cancer; unless there’s a family history, they should start getting screened at age 50.
Checking out symptoms
If you are experiencing symptoms described here, the Sanford Center for Digestive Health can work with you to find answers.
More digestive health stories
- Medical specialists publish guidance on C. diff prevention
- Food allergies increasingly common in children
- Health risks of acid reflux/gastroesophageal reflux
…
Posted In Digestive Health, Internal Medicine, Pathology, Symptom Management

