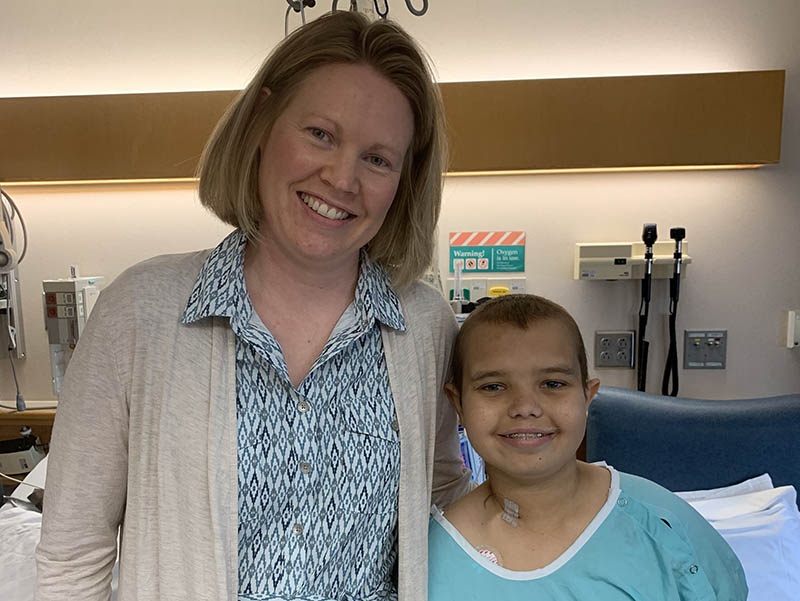
Jan Germundson and Ashton Hanson had one thing in common: spending their childhood in Williston, North Dakota.
Otherwise, Germundson is 40, and Ashton is 14. She’s a nurse in Sanford Medical Center Fargo’s neonatal intensive care unit (NICU). He’s a seventh-grader in a Williston middle school.
They’d never heard of each other before last summer, when Germundson read a news story about Ashton from her hometown newspaper.
And even then, it took another six months for Ashton to learn that a woman living with her husband and four children on the opposite end of North Dakota could soon radically change his life.
If everything worked out, a generous gift from Germundson would eliminate Ashton’s need to attach himself to a machine for 10 hours each night. The machine keeping him alive cleansed his blood in place of his diseased kidneys, which no longer could.
Sick since kindergarten
Ashton spent nearly all of elementary school coping with his kidney disease. He first got sick during the winter of his kindergarten year, with a fever that would go away only until a dose of Tylenol or Motrin wore off.
“I took him to the emergency room because I knew there was something wrong,” said Ashton’s mom, Melissa Lindvig.
A urinalysis revealed far too much protein. Further testing resulted in a referral to a pediatric nephrologist at Mayo Clinic.
Ashton’s initial diagnosis of minimal change disease, marked by excessive protein and treated by medication, changed when he relapsed about six months later. A kidney biopsy was done, determining his true diagnosis: a rare disease called focal segmental glomerulosclerosis (FSGS).
FSGS may have an identifiable cause, such as an infection or additional disease, or it may not, as in Ashton’s case. Either way, scarring occurs in the kidney when FSGS attacks and damages part of the kidney’s “filter system.” FSGS, and the scarring, can progress to the point of kidney failure.
Ashton also received a diagnosis of a heart murmur and left ventricle hypertrophy, where the walls of that part of the heart have thickened.
He was placed on steroids and other medication, as well as diet restrictions, and seemed to be responding well. But then in October 2017, he broke his big toe at school.
“We always thank him for breaking his toe,” Lindvig said. Without that, and preparations for the surgery that was scheduled to fix it, they wouldn’t have realized how much his FSGS had actually progressed.
Starting dialysis
In the process doing labs for his pre-op evaluation, Ashton’s Williston doctor sent the results to his nephrologist at Mayo. That doctor called and said Ashton needed to come to Mayo immediately. His kidney function had dropped to 12%, and starting dialysis was vital.
“I was scared,” Lindvig said. “We knew when he had FSGS that he would eventually need a kidney transplant, but depending on the time frame, we didn’t know when. It wasn’t until he broke his toe that we knew.”
Related: Transplant surgery care at Sanford Health
As for Ashton, Lindvig doesn’t know if he realized exactly what it all meant. “He just knew that there was something wrong with him, and he wasn’t a normal kid,” she said.
Ashton qualified for peritoneal dialysis, in which a machine helped cleanse his blood starting at 7:30 p.m. through a tube in his stomach. Confined to his bedroom each night, with his cat kept out for sanitary reasons, Ashton couldn’t go on a camping trip or to a sleepover at a friend’s house. If something went wrong with his machine — if it wasn’t draining properly, for example — an alarm would sound to wake him up, and he would make adjustments to it.
Lindvig was grateful Ashton could avoid a monthly medical journey to Rochester, a 15-hour drive one way when you allow for stops and for traffic around the Twin Cities. Instead, he was able to schedule his regular visits with nephrologist Michael LeBeau at Sanford Medical Center — Bismarck (who is now president of Sanford Health’s Bismarck region). That turned the monthly ordeal into a reasonable day trip.
Nevertheless, Ashton struggled with low energy. “He was tired a lot,” Lindvig said. “He would also fall asleep in class.”
Looking for a donor
Lindvig thought she had a great chance of being able to donate one of her kidneys to Ashton and end his illness. But an issue with a medication she took that had gone through her kidneys prevented her from being a match.
When she learned that she wouldn’t be able to give her son what he desperately needed, Lindvig “had no clue” about their chances of finding a living donor.
Local media, including the Williston newspaper, reported last year about Ashton seeking a kidney donor.
One local woman was willing and a match for Ashton, but her age made the medical team prefer considering her as a “paired donor” in a kidney swap if another appropriate donor-recipient pair could be found.
‘I could maybe do that’
Germundson grew up in Williston well before the Bakken oil patch turned it into the city with the fastest-growing economy in the nation in 2014. She estimates Williston had about 13,000 people — about half of its current size — when she grew up.
Germundson really wanted to be a NICU nurse, but Williston had no NICU. “So I knew I wasn’t going to be staying,” she said.
Beyond oral surgery to remove her wisdom teeth and eye surgery to correct her vision, Germundson hadn’t been through any surgeries herself. But she did know a couple of people who had had surgery to donate a kidney — one to a relative, one to a stranger.
So when a Williston newspaper’s Facebook post about Ashton’s plight caught her eye, she thought, “Hmm. I could maybe do that.” His blood type, listed in the article, was compatible with hers.
“He was pretty much the same age as my daughter,” Germundson said.
“If any of my kids needed dialysis and none of my family was able to donate, I would want somebody to come forward.”
So she submitted her information online and got a call back from Mayo Clinic in October 2018 explaining the process. They sent her a kit for having lab work drawn, which she sent back. But after that, she heard nothing and figured she wasn’t being considered. Then she received a call in February 2019 inviting her to come to Rochester for a couple days of further testing.
Germundson completed the testing and talks with social workers in March. The transplant panel then reviewed the results and said she still needed to complete a mammogram, given her age.
“Once that was done in May, then they said that yes, I was approved and cleared to donate,” she said.
‘I broke out in tears’
After Germundson made that March trip, Mayo encouraged her to get in touch with Ashton’s family and tell them she was willing to be a donor.
The only way Germundson could think of to contact Lindvig was through a Facebook message. But that was a hard message to write.
“I just told her that I had been thinking about it for a while, and that I had a daughter that was her son’s age, and that I just had been praying about it and thought that I should do this for them,” Germundson said.
Lindvig recalls receiving that life-changing note.
“When I got Jan’s Facebook message, I was sitting at home, and I broke out in tears,” she said. “Because it’s like, is this true? Is this really going to happen?”
“But,” Lindvig added, “I didn’t want to get my hopes up too much and then find out that it’s not going to happen. So from that point up until the 16th of July, I was a nervous wreck.”
July 16 was the planned date for Ashton’s kidney transplant. Even as Lindvig wondered whether the surgery would actually happen, she did everything she could to make sure Ashton would be ready. She watched what he ate. “If he had a sniffle, I was watching that.”
They had a scare six weeks before the transplant date when a staph infection developed around Ashton’s peritoneal dialysis tube. Fortunately, antibiotics cleared it up, and he remained on them until his surgery.
‘I know what it’s like to lose a loved one’
Meanwhile, the surgery was also very much on Germundson’s mind.
She asked a lot of questions of both people who had been through the process about two decades before — what recovery was like, for example, or if they noticed any resulting issues now.
“Neither one of them said that they regretted doing it or that they wouldn’t do it again,” Germundson said.
Still, the notion of going through an unnecessary surgery sent her mind on a roller coaster ride of sorts. “There was some weekends where I was like, am I really being crazy in doing this?” she said. Then at other times, she’d think, “OK, I’m doing this. It’ll be fine.”
A couple of things helped affirm her decision.
She stayed close to her faith, especially because she believed this was something she had been called to do. She prayed, read her Bible and kept this verse in mind, from Joshua 1:9: “Be strong and courageous. Do not be afraid. The Lord your God is with you wherever you go.”
And she was influenced by the deaths of her father and father-in-law in 2018. “I know what it’s like to lose a loved one,” she said. “So I just knew if I could somehow prevent somebody else from going through that, that I wanted to.”
Going through surgery
Surgery day came on a Tuesday. Germundson had arrived the day before as promised. Ashton had stayed healthy and arrived about 10 days before for evaluations made more extensive by his heart issues.
Lindvig said Ashton felt scared going into the surgery. And she felt nervous. “It was his last chance,” she said. “Because if the kidney didn’t take, that would probably have been the end. Otherwise, he would have been back on dialysis.”
The surgeon came to Germundson’s operating room first and removed her kidney within a half-hour or so. Then he went over to Ashton’s operating room and placed the kidney in his abdomen, on the right side, leaving his old kidneys in place higher up and further back. Ashton’s surgery, which involved connecting the new kidney to blood vessels and the bladder, took about four or five hours, Lindvig remembers.
“It really wasn’t too bad,” Germundson said of her surgery. “I couldn’t use my stomach muscles very much, but I really didn’t have hardly any pain at all.”
Germundson spent three nights in the hospital recovering. She was walking around the day after surgery, “and it just kept getting better each day,” she said.
Also the day after surgery, the surgeon brought Lindvig and her mother to meet Germundson for the first time. “They were very appreciative and were crying,” Germundson said.
‘A room of tears’
Ashton’s recovery in the hospital went well, too. The day of surgery, he walked from the bed to the chair in his room, then to the nurses station several feet outside of his room.
Two days after surgery, Germundson made the trip to Ashton’s hospital room to meet the boy she had just given a vital organ to.
“He just reminded me of my own kids,” Germundson said. “When we went into his room, he was in there playing video games.
“But it was exciting to see that he was doing good.”
Lindvig said Ashton gave Germundson a big hug and said thank you — a “hug-hug,” Ashton agreed.
“It was a room of tears,” Lindvig added.
Getting used to a kid with energy
Germundson took six weeks off work in the NICU to recover because she had restrictions on lifting for that long. She spent some of that time going on daily walks to prevent blood clots. She also napped frequently, having been forewarned she would feel tired. Her mom helped her for the first couple of weeks, when Germundson wasn’t able to drive yet.
Ashton and his mom, meanwhile, had expected to stay in Rochester for three months. After his discharge from the hospital July 22, they moved to the Ronald McDonald House and kept busy going to medical appointments. Ashton was placed on anti-rejection medication and antibiotics.
He recovered so well and had such good lab numbers, though, that Ashton was able to go home more than a month early.
And Ashton has been feeling great, Lindvig said. That’s something she wasn’t used to.
Before, “I would come home from work, and he would be in his room sleeping because he was exhausted,” she said.
Now, “he’s got more energy than I know what to do with.”
One thing he’ll never be able to use his newfound energy for: contact sports. His new kidney is protected from the back by his pelvic bone, but nothing really protects it from the front.
“He can do bowling, and then in April, he’ll start golf for school,” Lindvig said.
Ashton also looked forward to going camping, fishing and swimming — along with taking baths. He couldn’t submerge his peritoneal tube in water, so during dialysis, he had to take showers and give up the baths he enjoys.
One more child gets off the waiting list
Ashton’s diet has changed since dialysis. His sodium and potassium intake were very limited then. Now he can eat pretty much what he wants, while still watching the sodium and potassium to a certain extent.
“When I was on dialysis, the foods were kind of hard because everything at the store, the gas stations, Walmart, or something like that, that’s all sodium,” Ashton said. “We just had to figure out what we should have, and the hard thing was chicken nuggets.”
Has he had chicken nuggets since surgery? Oh, yes. Actually, Lindvig said, “he’s had pretty much everything that he could ask for.”
One thing he does have to be careful to avoid is eating any meat that’s even remotely raw, to prevent an infection. If he eats a hamburger or steak, it must be fully cooked — not pink inside. He can’t have lunch meat, either, unless it’s been cooked.
Ashton’s immune system is quite low, so he also has to try to avoid being around people who are sick. And there’s still a concern that the FSGS could attack Ashton’s new kidney, as it sometimes does in transplant recipients. So that will be monitored, along with his heart condition.
But after nine tough years, and especially after dialysis, life is really different now. Lindvig feels blessed that Ashton could get a new kidney when he did.
On Dec. 31, 2017, the same month Ashton started dialysis, 1,575 pediatric candidates were on the national waiting list for kidney transplants, according to the U.S. Department of Health & Human Services. During that year, 750 pediatric kidney transplants took place.
Thanks to Germundson, Ashton will be counted among that number of transplants at the end of 2019.
“To me,” Lindvig said, “she’s a perfect stranger that did a wonderful thing.”
More stories
- Woman marks 30 years of 3-times-a-week dialysis
- Researcher earns $1.9M grant to study kidney disease genes
- Kidney donor & recipient start as strangers, become friends
…
Posted In Children's, Dialysis, Fargo, General Surgery, Heart, Organ Donation, Pathology, Sanford Stories, Transplant