Even on her worst days, Tara Thom appreciated that it wasn’t obvious to anyone that she was ill. “I could still go out, and no one would know,” she said.
Thom was able to keep 85 percent of her hair during her battle with breast cancer. As the first patient to try cold cap therapy at Sanford Roger Maris Cancer Center, Thom found it effective and wanted others to have the opportunity as well.
“I had success, so I need to pass that along,” she said. With a focus on cold capping, Thom now mentors breast cancer patients through the My Survivor Mentor program.
Cold caps were invented in Europe in 1998, then made their way to the U.S. a few years later. Then Thom asked staff members at the cancer center to try it.
After her single mastectomy and a week before she was scheduled to start chemo, a family friend asked Thom’s husband if she was going to use cold caps. “I had never even heard of it,” Thom said. Feeling like she had nothing to lose, she decided to commit to the cold capping process.
Thom recalls the support Dr. Amit Panwalkar, her oncologist at Sanford Health, showed as he gave her an additional week to get her caps ready before starting chemo. Surprised but thrilled with the success, Thom is grateful she got to use cold caps and recommends them to others.
Cold capping: a particular process
Thom recalls capping as a detailed process that one would struggle to do alone. She is grateful for her daughter, Allie, for helping her through multiple capping sessions. Allie was 19 and attending Concordia College in Moorhead, Minnesota, at the time of her mother’s journey. She adjusted her class schedule as needed to commit to capping her mother.
The process took a full day and occurred every time Thom received a chemotherapy infusion. Capping began an hour before the infusion, took place during the entire infusion and lasted for a few hours after the infusion. Every patient’s treatment time may be different, but Thom’s sessions lasted roughly three hours. At the end of each treatment day, Thom had spent approximately eight hours capping.
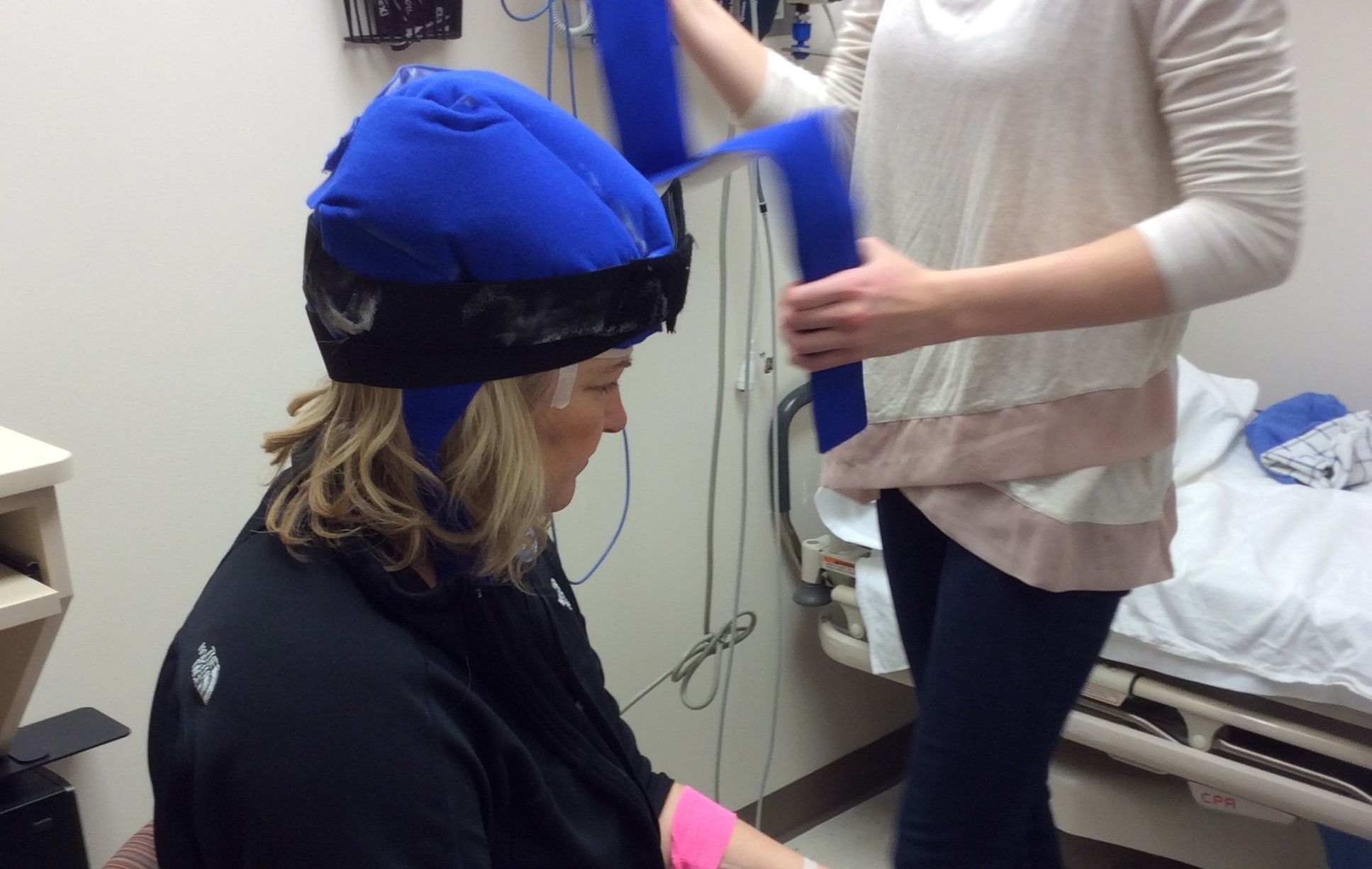
The cold cap fits tightly to the patient’s head and straps on like a helmet. Full of a Crylon Gel coolant, the hat chills to extremely cold temperaturess ranging from -15 to -40 degrees Fahrenheit. To reach those temperatures, the cap remains in a freezer until treatment time. It gradually thaws out during usage, which requires the constant cycling of multiple caps. Penguin Cold Caps, which is the brand Thom used, are made with medical grade hypo-allergenic plastics on the underside of the cap and have a blue nylon covering.
Allie Thom molded the caps to her mom’s head every three weeks. “Some people have it every week,” Tara Thom says. “It just depends on what your doctor implements for your drug regimen.”
She explains that the goal of cold capping is to freeze the hair follicles so they don’t absorb any chemotherapy drugs. Thom recalls the first time she and Allie used a cold cap. “I felt so terrible for my daughter,” she said. “We couldn’t get it to the right temperature, and she felt like she blew it.” The gel-packed freezing cap is supposed to be between -30 and -32 degrees Celsius, but it wouldn’t get colder than -26 for the first-time users.
“She did a fantastic job,” Thom said about her daughter. Patients typically lose the majority of their hair between the first and second infusions, she said, but she didn’t.
“At each infusion, I shouldn’t have had any hair, and I still had all of my hair, so then we knew it was working and Allie was doing it right,” she said. Thom kept a full head of hair throughout the process without any patches or bald spots. “It worked beautifully — totally successful,” she said.
Tips from Tara Thom
Thom happily shares tips to make sure everyone has the best possible chance of success with cold caps.
- Thom recommends Penguin cold caps. Penguin created the first cold cap and is the brand Thom recommends to her mentees. “I believe firmly in that system above all others, to be honest,” she says. Because it was the first, Thom believes it has evolved the most and is the most effective. Penguin’s website also has a lot of tips that she encourages mentees to use.
- It’s important to cover exposed skin. With the helmet-like object on her head, Thom says freezing exposed skin is very likely. Possible side effects of freezing skin include headaches, bleeding and blistering.
- Embrace the process. “You have to embrace the whole process and be faithful to what you’re doing,” she said. Thom stresses that it’s not for everyone as it requires a great deal of commitment and self-discipline. “If you don’t think you can, then it’s probably not for you, especially if you are hesitant and worried about the process,” she said. Thom thinks the best approach to cold capping is a “nothing to lose” attitude. There are no guarantees, so keeping an open mind is important.
- Be ready for the coldness. “The biggest and worst side effect is probably that you get so cold,” Thom said. “But once you’re numb on your scalp, you really don’t feel it.” When asked if it was painful or irritating, she said not at all. “It’s all external, nothing invasive. Once the cold cap is off, you warm up again. That’s the side effect.”
Mentoring other cold cap users
Although Thom has many tips for cold cap users, she believes the most beneficial thing she can give them is hope. “I have survived, so they have that hope of knowing another person that has made it through,” she said.
As a survivor herself, Thom understands the immense stress associated with fighting cancer. She focuses on providing empathy, comfort and listening ears in hopes of enhancing patients’ experience. “There are no guarantees or promises, but many people make it through,” she said. “And even though it feels like a lifetime during your journey, when you look back, it will be shorter than you ever thought it was.”
Thom has mentored at least a dozen people since beginning remission two and a half years ago. “I’m willing to share it all, because that’s what I’m here to do. I had success, so I need to pass that long,” she said. She has taught individuals and also a group of women in Sioux Falls who were interested in capping.
The My Survivor Mentor program wasn’t available during Thom’s journey, but she’s sure she would have used it if she had the chance. “Family can only do so much,” she said. “They don’t really understand the same way a mentor does.” Thom appreciates the ability for patients to connect with mentors who are not oncologists or family but outsiders who understand the inside.
Cold capping Q&A with Sanford nurse practitioner in oncology
Cold capping can be a complex and detailed process. It’s not for everyone, but many people find success from it. Sanford nurse practitioner in oncology Carrie Pfaff answers some commonly asked questions to help describe cold capping and its demands.
- Have you seen success with the cold caps? Yes. However, I would say most patients still experience some hair loss or hair thinning. The degree of hair loss varies depending on the chemotherapy administration regimen, the patient’s age and other comorbidities (sicknesses) he or she may have. Patients have told me their hair feels different, maybe more coarse and not as healthy. The majority of patients feel using the cold caps was worth it.
- Are cold caps common at Roger Maris Cancer Center? They are not common. I feel there are several reasons for this. One reason is that insurance doesn’t cover cold capping. Patients have to pay out-of-pocket for them, which isn’t an option for most patients. Also, patients are solely responsible for finding the type of cold cap they would like to use, make arrangements to get them here, along with bringing a support person to assist in using them before, after and during the treatment. Second, I feel that we as providers are not great about discussing it with patients, and again, there are several reasons for this. When a patient is first diagnosed, there is a lot of information to discuss and decisions to be made, which means cold caps are not high on the priority list in the grand scheme of things. However, I do think it is important for us as providers to at least give patients the information. That way they have the option to make an informed decision for themselves.
- Do you recommend cold caps? I feel that cold caps are a personal decision for each patient. When cancer patients receive a diagnosis, they experience so many emotions. Each patient processes their situation differently. But patients who express anxiety or emotional distress, specifically related to probable hair loss, I would definitely recommend it.
- Is there anything you’d like people to know about cold capping such as tips, advice or precautions? If a patient wants to pursue the use of cold caps, we will assist them in any way we can to help them accomplish their goal. I would like to see more use of them as I feel preventing alopecia (hair loss) helps patients with their mood, which has been proven to help decrease the side effects of treatment. More use will hopefully lead to more research and possibly insurance companies helping to cover the cost.
‘Treating the cancer comes first’
Thom says the hardest part of cold capping is accepting that not everyone can participate. Sometimes people only have four days’ notice, and that’s not much time to get your caps and set up the process.
“We’d love to get them more time before starting treatments, but treating the cancer comes first,” she said. Some patients have to travel and aren’t necessarily able to practically do it. And others aren’t able to because their drug regimen doesn’t allow cold capping.
Thom is fortunate that she was able to use cold caps and now appreciates the opportunity to help others. “I will share anything and everything to help others experience the same success I did,” she said.
More stories
- Breast reconstruction during mastectomy surgery
- Ways to help recover from chemo and how long it takes
- Cancer treatment can get in the way of an exercise routine
…